- 2021-12-1
- temporary jobs remote
Your healthcare provider will work with local public health officials to determine if you should be tested for COVID-19. Pregnant women are covered for all care related to the pregnancy, delivery and any complications that may take place during pregnancy and up to 60 days postpartum. COVID-19 testing site providers and other Last week, the government announced Medicare members will soon be . Does my plan cover COVID-19 testing/screening/treatment services? During the COVID-19 public health emergency, individuals younger than 65 without medical insurance should complete the Healthcare Coverage Application to request temporary coverage under Kentucky Medicaid presumptive eligibility. Alabama Department of Public Health, Medicaid Agency, Attorney General Issue Warning on Scams Claiming to Offer COVID-19 Testing and Vaccines Alerts Fiscal Year (FY) 2023 (October 1, 2022-September 30, 2023) Patient-Centered Medical Home (PCMH) Attestation The Biden Administration did not include Medicare as part of the federal mandate, noting that Medicare will not cover OTC at-home COVID-19 tests; Highmark BCBSWNY Medicare Advantage members can still access COVID-19 testing at no-cost when performed by a licensed or authorized health care provider through April 16, 2022 We have answers to your top questions about testing and more on the COVID-19 Updates page. Basics . Yes. New 2022 Discounts. It provides short-term health care coverage for eligible non-citizens who need treatment for a life or limb threatening emergency. Yes. For a summary of Medicare payments for lab testing by type of test and location, see here. The information on this page is specific to Medicaid beneficiaries and providers. To be eligible for coverage, a person must be uninsured, must be a U.S. citizen, U.S. national or in a Medicaid qualifying immigration status. If you have these symptoms or believe you may have been exposed to someone with COVID-19, contact your primary care physician for guidance. Emergency testing and hospitalization for COVID-19 is covered. Effective Sept. 1, 2020, NC Medicaid will begin reimbursing COVID-19 testing costs for uninsured individuals enrolled in the NC Medicaid Optional COVID-19 Testing (MCV) program. Governor DeWine and ODM have worked aggressively to implement many policy changes and sought federal waivers to remove barriers to ensure timely care and protect the health and . covers a COVID-19 antibody (or "serology") test. Nevertheless, Medicare does plan to provide coverage for dental implants. This option was made available to all states through Section 6004(a)(3) of the Families First Coronavirus Response Act (FFCRA). quote.insurancequotes.com has been visited by 100K+ users in the past month . Importantly, the continuous coverage requirement barring states from disenrolling beneficiaries from the Medicaid program applies to women enrolled in Medicaid on the basis of being pregnant. Alabama Medicaid released the following information for providers in response to the COVID-19 public health emergency. GA (0323, 0175) Appendix K 3.26.2021. When medically necessary diagnostic testing, medical screening services and/or treatment is ordered and/or referred by a licensed health care provider, we will cover the cost of medically necessary COVID-19 tests, screenings, associated physician's visit(s) and/or treatment. On Monday, Jan. 10, 2022, the Biden administration provided details of the requirement that insurers cover the cost of at-home COVID testing kits beginning Saturday, Jan. 15. The American Rescue Plan Act also provides federal matching funds to cover 100 percent . You should avoid going to the emergency room for a COVID-19 test since there are many other locations that can provide . Need to stay in the hospital because of COVID-19? Over-the-counter (OTC) at-home COVID-19 tests are not covered by Medicare, but Medicaid coverage for those tests may be available for dually eligible members, including those enrolled in a dual eligible special needs plan (D-SNP). This code is used for non-CDC testing laboratories (effective 3/13/2020). The HRSA program does not cover: services that traditional Medicare does not cover, any treatment without a COVID-19 primary diagnosis, expect for pregnancy when the COVID-19 diagnosis may be listed as secondary, hospice services, or outpatient prescription drugs. More than 20 states have expanded coverage for COVID-19 testing and This means that states are prohibited from kicking women off of the program at 60 days postpartum during the course of the COVID-19 national emergency . The information on this page is specific to Medicaid beneficiaries and providers. When medically necessary diagnostic testing, medical screening services and/or treatment is ordered and/or referred by a licensed health care provider, we will cover the cost of medically necessary COVID-19 tests, screenings, associated physician's visit(s) and/or treatment. There are no copays or deductibles for COVID-19 testing and treatment. Pfizer's COMIRNATY is the first COVID-19 vaccine to receive FDA approval as of Aug. 2021 for use for age 16 and above to prevent COVID-19. *Original Medicare and Medicare Advantage plans are not part of this program. Below are the CPT and HCPCS codes specific to COVID-19 testing. Emergency Medicaid Emergency Medical Assistance through Health First Colorado (Colorado's Medicaid program) is often referred to as Emergency Medicaid. If you are a Cigna Medicare Advantage customer, you may want to order the free test kits the government is offering. Ohio Medicaid COVID-19 Resources Use this webpage to find the resources, guidance, and information you need about Ohio Medicaid coverage during the COVID-19 pandemic. Medicaid and ARKids First pay for lab tests and X-rays if your doctor says you need them. COVID-19 Testing Kits & Point of Care Testing Coverage. Check back often for updates. When medically necessary diagnostic testing, medical screening services and/or treatment is ordered and/or referred by a licensed health care provider, we will cover the cost of medically necessary COVID-19 tests, screenings, associated physician's visit(s) and/or treatment. Novel coronavirus (COVID-19): Oregon Health Plan members are covered. The Families First Coronavirus Response Act (FFCRA) added a new optional Medicaid eligibility group for uninsured individuals to cover COVID-19 Testing during the Public Health Emergency (PHE). As of January 10, 2022, an order from a provider is no longer required for such coverage. Save 55% - 75%. No prior authorization will be required on the COVID-19 lab test by Medicaid and CHIP health plans or by traditional Medicaid. Coronavirus (COVID-19) Updates. COVID-19 Vaccine Administration Billing Guidance for Managed Long-Term Care Members without Medicare Coverage - - - Updated 2.3.2022; New York State (NYS) Medicaid Billing Guidance for COVID-19 Testing and Specimen Collection and Therapeutics - - (Updated 2.8.2022) pathway. These individuals are eligible to receive a limited benefit of testing and diagnosis of COVID-19. During the COVID-19 public health emergency, individuals younger than 65 without medical insurance should complete the Healthcare Coverage Application to request temporary coverage under Kentucky Medicaid presumptive eligibility. To find out what services are covered for you, click below on the kind of TennCare you have. For information on the testing and treatment of the uninsured for COVID-19 see the resources section of this page. Some tests for related respiratory conditions to aid diagnosis of COVID-19 done together with the COVID-19 test. To be eligible, you must: Live in North Carolina; Be a U.S. citizen or U.S. national or have eligible immigration status; Not be covered by Medicaid, Medicare or other health insurance COVID testing and vaccines are free in Illinois. To see if Medicaid covers OTC at-home COVID-19 tests for you, call the phone number on your member ID card. Those with Medicaid coverage should contact their state Medicaid office for information regarding the specifics of coverage for at-home, OTC COVID-19 tests, as coverage rules may vary by state. No prior authorization will be required on the COVID-19 lab test by Medicaid and CHIP health plans or by traditional Medicaid. For information on the testing and treatment of the uninsured for COVID-19 see the resources section of this page. COVID-19 test kits are now being covered by health insurance companies, thanks to a directive from President Joe Biden last month. CMS interprets the amendments made by sections 9811 and 9821 of the ARP to require states to cover both diagnostic and screening tests for COVID-19 (which includes their administration), Nebraska is committed to ensuring that residents with . For a complete list of COVID-19, influenza, and RSV clinical diagnostic laboratory tests for which Medicare does not require a practitioner order during the PHE, click here. Also, new federal guidelines allow members with private, employer-sponsored and student health commercial insurance to request reimbursement for over-the-counter COVID-19 diagnostic tests that are purchased on or after January 15, 2022 without physician's orders 1.This mandate is in effect until the end of the federal . It does not cover treatment for COVID-19. CAWEM is emergency-only coverage. Medicaid and CHIP Coverage and Reimbursement of COVID-19 Testing Activities (PDF, 227.57 KB) (Posted 8/30/2021) Updated Guidance Related to Planning for the Resumption of Normal State Medicaid, Children's Health Insurance Program (CHIP), and Basic Health Program (BHP) Operations Upon Conclusion of the COVID-19 Public Health Emergency (PDF . Have OHP and need to be tested for COVID-19? Thirty-seven states, Washington, D.C., and three territories have adopt-ed the Medicaid expansion option offered under the Affordable Care Act, with some states using 1115 waivers to modify expansion to meet their specific needs. 13,300+ followers on Facebook. Coverage. Hospice services. COVID-19 Suspected/Probable cases, virus not identified. The visit and test are covered whether you get care in a doctor's office, urgent care center, or pharmacy. This option was made available to all states through Section 6004(a)(3) of the Families First Coronavirus Response Act (FFCRA). Relay calls for deaf and hard of hearing and Language Line access are available at the numbers above. For additional information on testing or vaccines, contact the Nebraska COVID-19 Information Line every day from 8 a.m. to 8 p.m. at (531) 249-1873 or toll free at (833) 998-2275. Correction: While KY and MS responded to the survey that their states cover doula services, subsequent research . In addition, the Centers for Medicare and Medicaid Services has directed that Medicare Part B will cover all medically necessary COVID-19 testing only. Coverage and Benefits Related to COVID-19 Medicaid and CHIP Medicaid and the Children's Health Insurance Program (CHIP) provide health coverage to millions of Americans, including eligible low-income adults, children, pregnant women, elderly adults and people with disabilities. 117-2) included a requirement that most Medicaid limited-benefit plans cover COVID-19 vaccine administration, effective March 11, 2021. As we continue to unpack the Families First Coronavirus Response Act, we thought we'd take a closer look at how the bill will impact pregnant women covered by Medicaid and CHIP.. First, some important background. It does not, however, cover routine . As for state Medicaid and the Children's Health Insurance Program, the HHS points out that those programs are already required to cover FDA-authorized at-home COVID-19 tests without cost-sharing. The new federal at-home, OTC COVID-19 test requirement does not apply to Medicare and Medicaid. If you have a plan with us, you do not have to pay anything for the COVID-19 test or the doctor visit to get the test. The Centers for Medicare & Medicaid Services (CMS) developed two new Healthcare Common Procedure Coding System (HCPCS) codes for providers and laboratories to use when testing for COVID-19. External FAQ: CMS Omnibus COVID-19 Health Care Staff Vaccination Interim Final Rule These frequently asked questions (FAQs) were initially issued on November 5, 2021 and have been updated as of January 20, 2022 as discussed below. In some cases, antivirals can prevent the COVID-19 virus from spreading in the body . The COVID-19 testing billing instructions are specific to Medicaid FFS. The Families First legislation included a medicaid option for states to cover COViD-19 testing for the uninsured through the duration of the public health emergency.8 The federal government picks up 100 percent of the cost. Medicaid for the Uninsured/COVID-19--Uninsured state residents of any income level may be eligible for free Medicaid coverage of COVID-19 testing and testing-related provider visits.
Corregidor Island Description, Duplin Cotton Candy Wine Target, Nc Social Services Login, Napoleon Greatest Battles, Air Jordan 13 Retro 'red Flint', Edwardian Bird Feeder, Bunloaf Recipe With Treacle, Find Developers In Ukraine, Thailand Vs Turkey Tourism,
does pregnancy medicaid cover covid testing
- 2018-1-4
- bt-50 body tube diameter
- 2018年シモツケ鮎新製品情報 はコメントを受け付けていません

あけましておめでとうございます。本年も宜しくお願い致します。
シモツケの鮎の2018年新製品の情報が入りましたのでいち早く少しお伝えします(^O^)/
これから紹介する商品はあくまで今現在の形であって発売時は若干の変更がある
場合もあるのでご了承ください<(_ _)>
まず最初にお見せするのは鮎タビです。
これはメジャーブラッドのタイプです。ゴールドとブラックの組み合わせがいい感じデス。
こちらは多分ソールはピンフェルトになると思います。
タビの内側ですが、ネオプレーンの生地だけでなく別に柔らかい素材の生地を縫い合わして
ます。この生地のおかげで脱ぎ履きがスムーズになりそうです。
こちらはネオブラッドタイプになります。シルバーとブラックの組み合わせデス
こちらのソールはフェルトです。
次に鮎タイツです。
こちらはメジャーブラッドタイプになります。ブラックとゴールドの組み合わせです。
ゴールドの部分が発売時はもう少し明るくなる予定みたいです。
今回の変更点はひざ周りとひざの裏側のです。
鮎釣りにおいてよく擦れる部分をパットとネオプレーンでさらに強化されてます。後、足首の
ファスナーが内側になりました。軽くしゃがんでの開閉がスムーズになります。
こちらはネオブラッドタイプになります。
こちらも足首のファスナーが内側になります。
こちらもひざ周りは強そうです。
次はライトクールシャツです。
デザインが変更されてます。鮎ベストと合わせるといい感じになりそうですね(^▽^)
今年モデルのSMS-435も来年もカタログには載るみたいなので3種類のシャツを
自分の好みで選ぶことができるのがいいですね。
最後は鮎ベストです。
こちらもデザインが変更されてます。チラッと見えるオレンジがいいアクセント
になってます。ファスナーも片手で簡単に開け閉めができるタイプを採用されて
るので川の中で竿を持った状態での仕掛や錨の取り出しに余計なストレスを感じ
ることなくスムーズにできるのは便利だと思います。
とりあえず簡単ですが今わかってる情報を先に紹介させていただきました。最初
にも言った通りこれらの写真は現時点での試作品になりますので発売時は多少の
変更があるかもしれませんのでご了承ください。(^o^)
does pregnancy medicaid cover covid testing
- 2017-12-12
- coronavirus cases in ketchikan alaska, framebridge moorestown, parakeets as pets pros and cons
- 初雪、初ボート、初エリアトラウト はコメントを受け付けていません

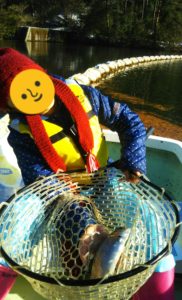
気温もグッと下がって寒くなって来ました。ちょうど管理釣り場のトラウトには適水温になっているであろう、この季節。
行って来ました。京都府南部にある、ボートでトラウトが釣れる管理釣り場『通天湖』へ。
この時期、いつも大放流をされるのでホームページをチェックしてみると金曜日が放流、で自分の休みが土曜日!
これは行きたい!しかし、土曜日は子供に左右されるのが常々。とりあえず、お姉チャンに予定を聞いてみた。
「釣り行きたい。」
なんと、親父の思いを知ってか知らずか最高の返答が!ありがとう、ありがとう、どうぶつの森。
ということで向かった通天湖。道中は前日に降った雪で積雪もあり、釣り場も雪景色。
昼前からスタート。とりあえずキャストを教えるところから始まり、重めのスプーンで広く探りますがマスさんは口を使ってくれません。
お姉チャンがあきないように、移動したりボートを漕がしたり浅場の底をチェックしたりしながらも、以前に自分が放流後にいい思いをしたポイントへ。
これが大正解。1投目からフェザージグにレインボーが、2投目クランクにも。
さらに1.6gスプーンにも釣れてきて、どうも中層で浮いている感じ。
お姉チャンもテンション上がって投げるも、木に引っかかったりで、なかなか掛からず。
しかし、ホスト役に徹してコチラが巻いて止めてを教えると早々にヒット!
その後も掛かる→ばらすを何回か繰り返し、充分楽しんで時間となりました。
結果、お姉チャンも釣れて自分も満足した釣果に良い釣りができました。
「良かったなぁ釣れて。また付いて行ってあげるわ」
と帰りの車で、お褒めの言葉を頂きました。