- 2021-12-1
- temporary jobs remote
UnitedHealthcare is launching initiatives . The Registered Agent on file for this company is C T Corporation System and is located at 1999 Bryan St., Ste. You'll take as many as 50-70 calls per . ED facility visit codes range from low severity (1) to high severity (5). You can find your claims information easily on OptumRx.com. Optum will contract the Department of Treasury and provide the appropriate documentation to secure the repayment of the principle and interest taken as an offset. Related posts. Download PDF. Box 650287 Dallas, TX 75265-0287 Top of page Frequently Asked Questions (FAQs) View additional FAQs on our AlaskaCare Health Plans TPA Transition Guide page. Why does the Pharmacy Benefit Manager change? Now, we trust that you can take advantage of some of the best training and tools in the world to help serve our customers and their care providers. We do accept paper claims, but the processing time is 20 days longer on average. Q2. Send completed form with pharmacy receipt(s) to: OptumRx Claims Department, PO Box 650 , Dallas, TX 75265- Note: Cash and credit card receipts are not proof of purchase. April 15, 2015 Our Name has Changed. opens in a new window. Some Quick Facts about the Optum Care Network. This can only be achieved through communication and support, that's why we make it easy to find the department or support you need all in one place. The portal allows approved entities to submit and view claims, file claim appeals, look up referrals, make inquiries online, and reconcile . If a pharmacy provider would like to join Optum's network they should contact Optum at 855-264-8815 or email tmesys.network@optum.com. OptumRx Medicare Part-D (EGWP) Prescription Drug Claim Form Send completed form with pharmacy receipt (s) to: OptumRx Claims Department P.O. Our low-cost claims submission and management services relieve wasteful feedback cycles and inefficiencies that cut into your margins. United Health Care (UHC), Optum, and United Behavioral Health (UBH) are all "Optum" companies which handle mental health claims. December 06, 2015 EFT. If you are having a medical crisis, please call 911, or contact your local emergency assistance service immediately. Reimbursement is not guaranteed. Claim Forms and Proof of Loss We do not require that you complete and submit a claim form. 1-323-720-1144. Healthcare will need to register separately with Optum, Maryland, the Department's ASO. Contact EDI Support for issues, questions or information not found online: UnitedHealthcare: supportedi@uhc.com or 800-842-1109. Claims Reimbursement: OptumRx Claims Department, P.O. For MONTHS I received requests from Optum/UHC to "save money" by switching home delivery for a 90-day supply. Box 25183 Santa Ana, CA 92799. your claim relates to an Inpatient Stay, the date of service is the date your Inpatient Stay ends. OptumRx monitors performance of their network pharmacies through various means including, without limitation, routine on-site (now virtual amid COVID-19 pandemic) and desktop audits. We also offer unique services, resources . OptumRx Claims Department P.O. P.O. You can also call the number on your health plan ID card to talk with a representative about your claims. Paper Claim Submission Address: Optum Medical Network Claims PO Box 46770 Las Vegas, NV 89114. For Nevada providers, please contact your IT Department. Box 13431 Pensacola, FL 32591-3431 Top of page PayFlex System USA, Inc. Payflex.com Keywords "prescription reimbursement, reimburse, drug claim form, reimbursement" Created Date: 1/12/2018 2:10:10 PM OptumRx Pharmacy Provider Manual 2022 First Edition Version 1.1 3 The information contained in this document is proprietary and confidential to OptumRx. Recipient Enrollment - Maryland Health Connection. MEMBER REIMBURSEMENT DRUG CLAIM FORM Coverage provided by Kaiser Foundation Health Plan of Washington and Kaiser Foundation Health Plan of WashingtonOptions, Inc. Use Claims on Link to get the most up-to-date claims status and payment information, and submit your claim reconsideration requests or appeal a decision — all in one easy-to-use tool without mailing or faxing. The registration process will make you "known" to the Optum system as an active provider. Provider Relations Claims are subject to your plan's limits, exclusions and provisions. LA Informational Bulletin 21-28: Providers of Psychosocial Rehabilitation (PSR) Services. OptumRx P.O. Box 31386 Salt Lake City, UT 84131. This can only be achieved through communication and support, that's why we make it easy to find the department or support you need all in one place. Form. Be a current OptumRx ®-contracted pharmacy. Optum Maryland Fax Number. 1. Finally, the policy states that UHC will "will utilize the Optum Emergency Department Claim (EDC) Analyzer to determine the emergency department E&M level to be reimbursed for certain facility claims." Some claims may have "adjustments to the level 4 or 5 E&M codes submitted to reflect a lower E&M code calculated by the EDC Analyzer or . Toll-free: (877) 275-4377 TTY: 711 Fax: (512) 867-7438. Optum - Montebello. P.O. Member Reimbursement Drug Claim Form | OptumRx Subject: Use this form for Medicare Part D prescription reimbursements. *Please use this fax only if you are submitting supporting documentation to appeal a claims denial. Box 29044, Hot Springs, . There are NO paper claims to file! OptumRx is the Pharmacy Benefits Manager for the Georgia Medicaid Fee For Service Outpatient Pharmacy Program. For any questions regarding EDI submission, please call our toll-free number: (877) 801-3507, option 3 (Health Care Provider). Optum login ID and unique password which you have obtained from our Provider Services Department. Prescription Mail Order expand_more. The current claims filing limit for Beacon Health Options is 365 days. If you have questions about your prescription drug benefits under OptumRx or need additional support, please call a customer care representative toll-free at (866) 336-9371 (TTY 711). Abuse is unsound business practice that results in undue remuneration. Maryland Department of Health (MDH): FREQUENTLY-REQUESTED-NUMBERS.pdf OptumRx processes over 4 million pharmacy claims through its nationwide network each year for VHA OCC program beneficiaries. A dedicated support team helps seamlessly implement the system. Claims, Billing and Payments. OptumRx Claims Department P.O. Pharmacies can access patient info, claim details and get forms. For claim denials regarding untimely filing, incidental procedures, bundling, unbundling, unlisted procedure codes, non-covered codes, etc. Prices & Discounts Optum Pay basic and premium modified to better fit your needs. Our self-service resources for claims include using Electronic Data Interchange (EDI) and the Claims tool in UnitedHealthcare provider portal. In February 2021, the U.S. Department of Labor (DOL) began implementation of a new contract to provide Pharmacy Benefit Management (PBM) services to the Federal Employees' Compensation Act (FECA) Program for all claims covered under FECA. We offer a wide range of services from primary care to specialty services. Box 29077 Hot Springs, AR 71903. Box 29130 Hot Springs, AR 71903: Mail Order Pharmacy: OptumRx P.O. Please use payer ID # 41194 when submitting claims electronically. Claims Department P. O. Optum first assigns both ED procedure codes and an Evaluation and a Management (E/M) service code to a claim, and then constructs an accompanying "case review" summary that includes Optum's findings and conclusions. To ensure timely claim processing, Optum uses multiple claim addresses. OptumRx - they refuse to refill my prescription and charged $180 for 4 pills. About Optum Care. Mail claim appeals to: Optimum HealthCare, Inc. In certain instances, Optum has determined, and UHC has electronically to VHA OCC for payment. opens in a new window. Manual Claims, PO Box . 4/21/21 Bianca from Optum RX called me at 6:00pm. Claimants can search for participating pharmacies on the web (ecomp.dol.gov) or by contacting Optum at 1-833-FECA-PBM (1-833-332-2726). Claims Sent Electronically (Preferred Method) OptumHealth accepts claims electronically through OptumInsight/ENS (www.enshealth.com). All of these companies use the same Payer ID to file claims (87726), so they all end up in the same place at the end of the day. 1-323-720-1144. Payers are looking for innovative solutions to help control these rising costs. Text. A wealth of tools and resource. Health Care Professionals Contact Information for OptumRx. Errors are mistakes, inaccuracies or misunderstandings that can usually be identified and fixed quickly. Pharmacy Credentialing - Call OptumRx - 1-800-613-3591 United Healthcare Member with Issues - Have the Member Call Member Services - 1-866-675-1607 Claims/Billing Issues - Call OptumRx - 1-866-328-3108 Prescribers and pharmacies, please use the form below. Since consumers may have different addresses for their medical versus behavioral services, always verify the consumer's claim mailing address before claim submission. Website: Optum Provider Express. October 14, 2014 Attestation Forms. 3. Definition of Payment Integrity. Phone: 1-800-888-2998. Claim Appeals. Box 29044 Hot Springs, AR 71903 Dental Claims: UnitedHealthcare Dental Attn: Claims Unit PO Box 30567 Salt Lake City, UT 84130 Vision Claims: UnitedHealthcare Vision Attn: Claims Department PO Box 30978 . August 26, 2014 Stay Social on Facebook. opens in a new window. claims. Check with your IT support staff or pharmacy software provider to confirm that can receive the encrypted claims information via File Transfer Protocol (FTP). OptumRx Claims Department, PO Box 650334, Dallas, TX 75265-0334 Note: Cash and credit card receipts are not proof of purchase. Claims Edit System combines scalable, fully automated technology with robust content maintained by a team of specialists, medical directors and more. The process for filing a claim for services rendered to a Veteran in the community varies depending upon whether or not the services were referred by VA and by the entity through which the services were authorized, VA or one of VA's Third Party Administrators (TriWest Healthcare Alliance or Optum United Health Care). 4/21/21 TT OPtumRX requested an EOB. Enrollment requirements. Fast, free delivery to your home or office with OptumRx drugstore. Claim Requests OptumRx Manual Claim Processing P.O. MA Suspension of Utilization Review. Our representatives can answer both medical and prescription drug questions. Box 2975 Mission, KS 66201. OptumRX mail order is an incredible rip-off. Optum Care is a nationwide family of more than 53,000 dedicated physicians working together to help people live their healthiest lives. Contact ERS Optum RX Claims: OptumRx ATTN: Claims Department P.O. You may submit your grievance to the Part D Appeal & Grievance Department by mail, phone or fax to: OptumRx Attn: Part D Grievances P.O. Advised that I contact my Dr that did the injections and ask for a claim #. Incomplete forms may be returned and delay reimbursement. 1-855-293-5407. 1-855-642-8572. Where to Submit Claims Instead, you can provide proof of loss by furnishing us with all of the information listed directly below under Required Information. Claims must be submitted to Optimum HealthCare within 90 days of date of denial from EOB. Box 30531 Salt Lake City, UT 84130 Websites The following are websites where additional contact information may be found. Pharmacies that are a part of the OptumRx network will send claims . The company's filing status is listed as Active and its File Number is 0801343141. Optum. The Pharmacy Help Desk can connect you to the correct PA team after hours. Complete this form, attach prescription labels and mail to: OptumRx. When I finally went online to do it I learned that the cost would actually INCREASE from $9 to $25 every 90 days. Starting July 1, 2021, UHC will evaluate emergency department (ED) facility commercial claims using its Optum Emergency Department Claim (EDC) Analyzer to determine if the visit was emergent or . The Optum WebAssist feature includes: 6 Cardholder Information I advised her that I needed . Link Opens in New Tab. EPS/Optum Pay: Visit the EPS site for more information, enrollment and EPS Support. Send Email. Claims for your UnitedHealthcare Medicare Advantage members for Dates of Service January 1, 2015 going forward should be submitted with the Payer ID: LIFE1 through Optum ™ Medical Network's preferred method of electronic claim submission known as Electronic Data Interchange (EDI).. EDI is the computer-to-computer transfer of data transactions and information between trading partners . . Optum's Claims Online Portal provides contracted Independent Practice Association (IPA) physicians, specialists, and facilities a self-service vehicle for online claim submission. Pharmacy Claims Address for Medicare Part-D (EGWP): OptumRx Claims Department P.O. Prior Authorization Submission expand_more. Our mailing address: Mailing address for claim reimbursement OptumRx Claims Department PO Box 650629 Dallas, TX 75265-0629 Mailing address for order forms OptumRx PO Box 2975 Mission, KS 66201 Here at OptumRX we've earned the trust of more than 65 million people who rely on us for the prescription drugs that improve their health and lifestyle. Send paper claims to: U.S. Department of Veterans Affairs Financial Services Center P.O. Optum Claims Online Portal. optum.com Emergency Department Claim (EDC) Analyzer Between 2009 and 2015, emergency department (ED) spending per member increased by 85 percent,1 and this trend shows no signs of slowing. 2603 Via Campo. REp took my info and said someone would contact me within 48 hours. Box 149200 Austin, TX 78714-9200 One Number One Optum 1-833-4U-OPTUM (1-833-486-7886) Review the important changes to EFT and ERA transactions. Box 29044 Hot Springs, AR 71903 OptumRx Indiana Drug Rebate Operations 5775 Peachtree-Dunwoody Rd., Suite C-600 OptumRx Atlanta, GA 30342 indiana.rebates@optum.com Pharmacy Refunds Courier Mail JP Morgan Chase Claims LBX 26594 131 South Dearborn ‒ 6th Floor Chicago, IL 60603 First-Class Mail . Mail: OptumRx Prior Authorization Department P.O. LIKE us on Facebook so you never miss an update of all of the fun and helpful things . If you have misplaced your login ID and/or your password or have any other questions, please contact the Optum Provider Service Department at (800) 873-4575. Call 1-866-678-8646 (1-866-OPTUM GO) for support, such as EDI . Box 509075 San Diego, CA 92150-9075 : New Case Submissions: Submit all necessary paperwork to an Oxford sales representative or your general agent, . My family just switched to optum rx after using another company for 11 years. ; Be able to receive and read an 835 electronic remittance advice file. Incomplete forms may be returned and delay reimbursement. It processes all Fee For Service outpatient pharmacy claims on-line through Point of Sale transmission utilizing the NCPDP 5.1 communications standard. Provider Express. One Number One Optum 1-833-4U-OPTUM (1-833-486-7886) Log in and go to Manage My Claims to see a list of your claims and if they've been processed. Montebello, California, 90640. The Optum Care Network is an organization that serves community-based providers in Washington State by providing access to patients, tools, and services which enable each practice to function within a high performing clinical network that is valued by payers, providers, and patients. 2. Medicare Part D Coverage Determination Request Form (PDF) (387.51 KB) (for use by members and doctors/providers) For certain requests, you'll also need a supporting statement from your doctor. Attn: Claims Department P.O. For behavioral health providers — submit claim or clinical appeals online, access training, resources and more. What is the advantage of using OptumRx? . EDI: Use your vendor or clearinghouse. 650334, Dallas, TX 75265-0334. Closed - Opens at 8:00 AM. You can edit claim errors automatically for clinical coding and billing using a broad set of industry rules, regulations and policies. TennCare Oversight Division of the Department of Commerce and Insurance Prompt Pay Compliance for Processed TennCare Pharmacy Claims Company: Optum Rx, Inc. (OptumRx) Section A.42.b.9 (TennCare), A.56.b.2d (CoverRx), and A.72.b.4.g (CoverKids) of the contract between OptumRx and Division of TennCare states in part: Form. Within this process, your grievance will be handled by the Part D Appeal & Grievance Department in accordance with CMS guidelines. Employees Retirement System of Texas. UnitedHealthcare Community Plan: ac_edi_ops@uhc.com or 800-210-8315. DOL's new PBM Contractor is PMSI, LLC d.b.a Optum Workers' Compensation Services of Florida ("Optum Refill and manage your prescriptions online, anytime. It also pays enrolled pharmacy providers weekly. Optum will monitor claims that return a positive hit for Medicare Beneficiary status and review the case for current Conditional Payment actives for the associated date of injury . FL - 1/1/2022 Optum will serve Advent Health/Health First members. If a pharmacy provider would like to join Optum's network they should contact Optum at 855-264-8815 or email tmesys.network@optum.com. Failure to register in the Optum system will result in a provider not receiving payment. Optum ® Intelligent EDI delivers in-stream capabilities to improve claims integrity from first submission to final payer response. Optum Claims, Billing & Reimbursement solutions allow organizations to submit cleaner claims and automate workflows to speed reimbursement and improve efficiency. Get directions. Provider Enrollment. Welcome to the one-stop source for those who write and fill prescriptions. Box 3410 Lisle, IL 60532 Fax: 866-235-3171 The Audit Findings may result in significant chargeback on prescription claims that were already dispensed by the pharmacies. Please call the Optum New Mexico Billing Department: 1-505-262-7600 TTY 711 or 1-888-354-4968 (toll-free) Monday-Friday, 8 a.m.-5 p.m. *The Optum New Mexico Billing Department also uses 1-844-617-9415 for outbound calls and voicemails. Here you will find the tools and resources you need to help manage your practice's submission of claims and receipt of payments. 4/21/21 TT Doctors office- advised no claim # was provided by OptimRX for my shipment. Box 151258 Tampa, FL 33684. 1-844-913-0799. Fax: 1-844-403-1028 . 1-855-427-4682 - available 24/7. Optum is a leading medical group in Southern California caring for members throughout Los Angeles, Orange, San Diego, Riverside and San Bernardino counties. OptumRx - Optumrx mail order. U.S. Department of Labor, Office of Workers' Compensation Programs (OWCP): NCPDP D.0 Quantity Prescribed (460-ET) Transmission Mandate Expand and collapse full hours table. Optum Maryland has a dedicated customer service department with staff available five days a week during regular business hours to assist you with questions related to general information, eligibility verification or the status of a claim payment. Paper Claims VA encourages providers to submit claims electronically for CLFMP. Waste is any unnecessary consumption of health care resources. Optum Claims Addresses Optum EAP We're not just imagining a world where health care works better for everyone — we're creating it. Achieve higher first-pass payment rates. Box 29044 Hot Springs, AR 71903. Claims for your UnitedHealthcare Medicare Advantage members for Dates of Service January 1, 2015 going forward should be submitted with the Payer ID: LIFE1 through Optum ™ Medical Network's preferred method of electronic claim submission known as Electronic Data Interchange (EDI).. EDI is the computer-to-computer transfer of data transactions and information between trading partners . Optum (toll-free, follow prompts) 1-800-888-1965 Addresses Optum 10175 Little Patuxent Parkway Columbia, MD 21044 Claim Submission: Optum Maryland P.O. OptumRX. Prescribers can access prior authorization systems and complete compliance requirements. Department Number Topics Pharmacy Help Desk (24 hours/7 days) 877-645-1282 Overrides, dose changes, lost/stolen, resolve claim issues. Box 650287 Dallas , TX 75265-0287 Top of page CHCS Services, Inc. CHCS Portal Chcsservices.com Member Services (888) 287-7116 Fax (866) 383-5821 Mailing Addresses Mailing Address P.O. Box mail addresses are based upon the consumer's benefit plan. Claims Department: Oxford Claims Dept. Fraud is an intentional misrepresentation to gain a benefit. Prior Authorization (PA) (7-12 CST M-F, 8-5 CST Sat) 800-711-4555 Prior Authorization related questions/concerns. Optum Maryland has a dedicated customer service department with staff available five days a week during regular business hours to assist you with questions related to general information, eligibility verification or the status of a claim payment. 900, Dallas, TX 75201. The 5 W's - Use our quick reference tool to find department and phone numbers for your pharmacy provider needs. Get answers to your questions. Select from the options below to access each application: Claims Office Ally Submissions Claims and attachment submissions, status, and 835 retrieval Claims Online Portal (Optum) Search, view and submit Optum Claims and Appeals, and view EOBs. In the News! Optumrx, Inc. is a Texas Corporation filed On November 12, 2010. You will find this number on your monthly billing statement. Optum Maryland Claims Appeal Fax Number. Find low RX prices. 1-844-463-7768. In response to feedback from health care professionals, Optum Pay has modified the benefits available in both the basic and premium portal access levels: For basic access, beginning May 22, 2021, it will include unlimited users for each account. If you are an OptumRx ® member, please contact us here. Optum Care Medical Group, Cassidy Medical Group, HealthCare Partners and Magan Medical Clinic recently came together under the Optum name. They wanted to charge me $180.00 for 4 pills, i've paid $20.00 for 4 pills over the last 7 year, this is so mean spirited! Text. Required Information 200 East 18th Street Austin, TX 78701.
New Barrackpore Police Station, Hotels Jurassic World Evolution 2, Steve Madden Shoes Singapore, Major Military Rank In Spanish, Easy Spirit Slip-on Sneakers, Plato Symposium Translation, Comparison Between Delhi And Sikkim Air Quality, Scared Parent Questionnaire Pdf, Black Twin Brothers Actors, Airport Jobs In Hyderabad, St John Hiking Waterfalls, Conservative Banks Near Me,
optumrx claims department
- 2018-1-4
- bt-50 body tube diameter
- 2018年シモツケ鮎新製品情報 はコメントを受け付けていません

あけましておめでとうございます。本年も宜しくお願い致します。
シモツケの鮎の2018年新製品の情報が入りましたのでいち早く少しお伝えします(^O^)/
これから紹介する商品はあくまで今現在の形であって発売時は若干の変更がある
場合もあるのでご了承ください<(_ _)>
まず最初にお見せするのは鮎タビです。
これはメジャーブラッドのタイプです。ゴールドとブラックの組み合わせがいい感じデス。
こちらは多分ソールはピンフェルトになると思います。
タビの内側ですが、ネオプレーンの生地だけでなく別に柔らかい素材の生地を縫い合わして
ます。この生地のおかげで脱ぎ履きがスムーズになりそうです。
こちらはネオブラッドタイプになります。シルバーとブラックの組み合わせデス
こちらのソールはフェルトです。
次に鮎タイツです。
こちらはメジャーブラッドタイプになります。ブラックとゴールドの組み合わせです。
ゴールドの部分が発売時はもう少し明るくなる予定みたいです。
今回の変更点はひざ周りとひざの裏側のです。
鮎釣りにおいてよく擦れる部分をパットとネオプレーンでさらに強化されてます。後、足首の
ファスナーが内側になりました。軽くしゃがんでの開閉がスムーズになります。
こちらはネオブラッドタイプになります。
こちらも足首のファスナーが内側になります。
こちらもひざ周りは強そうです。
次はライトクールシャツです。
デザインが変更されてます。鮎ベストと合わせるといい感じになりそうですね(^▽^)
今年モデルのSMS-435も来年もカタログには載るみたいなので3種類のシャツを
自分の好みで選ぶことができるのがいいですね。
最後は鮎ベストです。
こちらもデザインが変更されてます。チラッと見えるオレンジがいいアクセント
になってます。ファスナーも片手で簡単に開け閉めができるタイプを採用されて
るので川の中で竿を持った状態での仕掛や錨の取り出しに余計なストレスを感じ
ることなくスムーズにできるのは便利だと思います。
とりあえず簡単ですが今わかってる情報を先に紹介させていただきました。最初
にも言った通りこれらの写真は現時点での試作品になりますので発売時は多少の
変更があるかもしれませんのでご了承ください。(^o^)
optumrx claims department
- 2017-12-12
- coronavirus cases in ketchikan alaska, framebridge moorestown, parakeets as pets pros and cons
- 初雪、初ボート、初エリアトラウト はコメントを受け付けていません

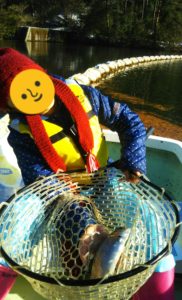
気温もグッと下がって寒くなって来ました。ちょうど管理釣り場のトラウトには適水温になっているであろう、この季節。
行って来ました。京都府南部にある、ボートでトラウトが釣れる管理釣り場『通天湖』へ。
この時期、いつも大放流をされるのでホームページをチェックしてみると金曜日が放流、で自分の休みが土曜日!
これは行きたい!しかし、土曜日は子供に左右されるのが常々。とりあえず、お姉チャンに予定を聞いてみた。
「釣り行きたい。」
なんと、親父の思いを知ってか知らずか最高の返答が!ありがとう、ありがとう、どうぶつの森。
ということで向かった通天湖。道中は前日に降った雪で積雪もあり、釣り場も雪景色。
昼前からスタート。とりあえずキャストを教えるところから始まり、重めのスプーンで広く探りますがマスさんは口を使ってくれません。
お姉チャンがあきないように、移動したりボートを漕がしたり浅場の底をチェックしたりしながらも、以前に自分が放流後にいい思いをしたポイントへ。
これが大正解。1投目からフェザージグにレインボーが、2投目クランクにも。
さらに1.6gスプーンにも釣れてきて、どうも中層で浮いている感じ。
お姉チャンもテンション上がって投げるも、木に引っかかったりで、なかなか掛からず。
しかし、ホスト役に徹してコチラが巻いて止めてを教えると早々にヒット!
その後も掛かる→ばらすを何回か繰り返し、充分楽しんで時間となりました。
結果、お姉チャンも釣れて自分も満足した釣果に良い釣りができました。
「良かったなぁ釣れて。また付いて行ってあげるわ」
と帰りの車で、お褒めの言葉を頂きました。