- 2021-12-1
- temporary jobs remote
Click each category below to access relevant forms. CMS-1450 (UB-04) Roster bill for patients (find your MAC website to learn more about or set up roster billing) Professional How to Submit Professional Claims. Completing the Pharmacy Paper Claim Form. Louisiana Healthcare Connections Member with Issues - Have the Member Call Member Services - 1-866-595-8133. ONE FORM PER PATIENT PER PROVIDER Please print clearly, complete all applicable sections and sign. Completed CMS-1500 claim forms should be . Pseudo-DIN List. - Press 5 if your call is regarding pharmacy claims processing for the Conduent customer service helpdesk and follow the prompts, or you may call Conduent directly at 1-800-884-3222. For additional claim preparation information, refer to the Forms: Legibility and Completion Standards section of this manual. Fill out and return the attached prescription drug claim form. Completing claim forms. Pharmacy Documentation Requirements 159. Prior Authorization Forms. 261.000 Introduction to Billing 7-1-20 For paper billing of non-NCPDP claims (including immunosuppressant drug crossover claims or vaccine claims), pharmacy providers use the CMS-1500 form to bill the Arkansas Medicaid Program for services provided to eligible Medicaid beneficiaries. Medical Billers and Coders July 13, 2018. The Billing & Reimbursement section is designated for information pertaining to claims, billing, and reimbursement information and changes. Plan Member Documents. Claim attachment (use when sending supporting documents to a non-pharmacy claim) Pharmacy claim attachment (use when sending supporting documents to a pharmacy claim) You and your office staff can stay up-to-date on topics including clean claims, proper coding for disbursements, remittances, and specific billing procedures. Therefore, the NPI of the Medicare provider (i.e. NCPDP's Elite Partners provide the highest level of . For additional claim preparation information, refer to the Forms: Legibility and Completion Standards section of this manual. Obtain your National Provider Identifi er number (NPI). Pharmacy providers billing directions for COVID-19 vaccines via NCPDP D.0 pharmacy claims. Field 1 OTHER COVERAGE CODE Not required Complete 'OTHER COVERAGE CODE' using To reverse a claim . What we need to process your payment. Worker's name Worker's legal name in the last, first, middle initial format. - the purpose of the DAW code is to describe why the generic form of the dug or brand form was dispensed. In this example, a pharmacy is billing for a pediatric/female catheter prescribed for a CCS client. Pharmacy Billing Process Pharmacy claim submission: • When pharmacy claim is transmitted, it does so through a switch vendor, which is a vendor that ensures the information being transmitted to conform to the National Council for Prescription Drug Programs (NCPDP) standards prior to the claim reaching the Pharmacy Benefit Manger (PBM) •Providers billing a B DMEMAC for prescription drugs furnished by a retail pharmacy must comply with the National Council for Prescription Drug Programs (NCPDP) Telecommunications Standard D.0 and Batch Standard Version 1.2. . The ordering and rendering provider(s) must be registered with AHCCCS. See the special instructions for compound drug claims following the regular instructions. About > Solutions. Completing claim forms. Under Your Plan Forms, look for Pharmacy claims. Administrative Forms. Our self-service resources for claims include using Electronic Data Interchange (EDI) and the Claims tool in UnitedHealthcare provider portal. For a list of services carved out of the managed care programs, see the Member Eligibility and Benefit Coverage module. − See Section 9.0 - Appendix A - Universal Claim Form for sample UCF and instructions. Billing Tips: Quantities must be in . Please submit all documents to: Providence Health Plans Attn: Claims Processing P.O. Paper Claim Forms • (• • • • and processing. The Universal Claim Form or the Workers' Compensation/Property and Casualty Universal Claim Form are to be sent to the insurer/payer/health plan for the patient/member. Pharmacy: division form DWC-066; Dental: (ADA) Dental Claim form; Electronic medical billing. Pathway 1: Completion of PTCB-Recognized Education/Training Program for the Billing and Reimbursement Certificate and at least 6 months of experience as a pharmacy technician. State Medicaid agencies may provide different guidance. onto their . - Dispense as written (DAW) codes are submitted as part of third part claim. http://pharmacy.medicaid.ohio.gov/pharmacy-billing-information Paper (Manual) Manual claims follow the same business rules and edits as online claims. TennCare Provider Billing Manual for Professional Medicare Crossover Claims 4.0 1 . . The. entered on the CMS 1500 claim form, in the 837P format or Pharmacy POS formats. Medicaid Provider Portal. Field 1 Beneficiary Last Name. Provider Claim Appeal form will be available and must be completed and sent to the Medi-Cal Rx vendor via fax or mail. The C774 Pharmacy Prescription Invoice details these requirements; however, an electronically N/A GROUP I.D. The following are the four separate forms used for California workers' comp billing: Form CMS-1500 is for use by healthcare providers. Claims may be submitted electronically or the provider may log onto their Medicaid Provider Portal. Claims may be submitted electronically or the provider may log onto their Medicaid Provider Portal. MANAGED CARE HEALTH PLAN PHARMACY "CARVE OUT" Pharmacies may use the CMS-1500 claim form when billing Medicaid for these vaccines. submit claims through their pharmacy claims platform. Specialized Forms/Questionnaires. Download and complete the Patient claim for refund Pharmaceutical Benefits Scheme (PBS) form. Claim Sample-Pharmacy Version 4.0 . Professional Paper Claim Form (CMS-1500) . Provider Manual (Section 18.5 - Provider Claim(s) Appeal Forms) Universal Claim Form . Each claim may contain charges for only one (1) beneficiary. Health Benefits Claim Form. a registered pharmacy or a recognized provider's offi ce, such as a physician's offi ce (incident to the physician billing). Forms: Legibility and Completion Standards. Restrictions 160. The C774 Pharmacy Prescription Invoice details these requirements; however, an electronically Once you've found your form you can download it in PDF format using the "download" link. Click here for instructions on accessing your form. Submit pharmacy bills via paper billing form: Use the Statement for Pharmacy Services form for single drugs with NDCs. Mail or fax the claim form and the original receipt for processing. Linkages between Purchases & Billing: Most hospitals have separate processes to order drugs, administer them, and process reimbursement. 1 If in doubt of which claim format to use, contact Provider Services at 800-336-6016, or refer to your provider guidelines. field (Box 19) of the claim, type it on an universal claim form pharmacy. Refer to the Compound Pharmacy Claim Form (30-4) Completion section of this manual for instructions to complete claim fields not explained in the following examples. 8. laims may be submitted electronically if the pharmacy's vendor software can code and transmit an 837P X12 claim. Claim Form This form may be used for Health Net Medicare products. Non-Ontario Drug Benefit Eligible Recipients 160. 2.2 Media Options POS If the billing provider has multiple locations but a single NPI, enter the zip code of the location where the service was rendered so the correct billing provider can be identified. Please submit a separate claim form for each patient and pharmacy from which you purchase medications. You can use this form to claim a refund if either you: didn't show your Medicare card or concession card when you purchased the medicine at the pharmacy. Paper Claims. , , and You must obtain prior authorization or risk non-payment. Fields 24A through 24J apply to each billed line. Required Enter the recipient's 13 digit Medicaid ID. claim form - Multiple claim lines from more than one MRN for the same recipient on one . Not required N/A NAME Not required N/A PLAN NAME Not required N/A PATIENT NAME Required Enter the Recipient's full name: First, Last. 7. Box 52136, Phoenix, AZ 85072-2136 123456789 JOHN Q SAMPLE . Professional Paper Claim Form (CMS-1500) . For paper claim submission s for compounds, bill only one compound prescription per paper claim; do not mix compound claims with noncompound claims. UB-04 (CMS 1450) is a claim form used by hospitals, nursing facilities, in -patient, and other facility providers. Billing Guidance for Paper Claim Submission To be reimbursed for the administration fee when billing on a paper claim (Pharmacy Claim Form [30-1] or Universal Claim Form), pharmacy providers must submit the claim with the NDC and the billing quantity as identified in the table above. The purpose of this notice is to update the COVID-19 vaccine administration fees for pharmacy providers to 100% of Medicare rates. NCPDP Basic Guide To Standards. The following claim form field information applies both to the Pharmacy Claim Form (30-1) and the Compound Drug Pharmacy Claim Form (30-4). A completed form must not be sent to NCPDP. 7.4 Filing Dental Claims 8. Field Name Entry Description N/A I.D. * Keep a copy of all documents submitted for your records. The provider's phone number is optional. Retain a copy for personal records. Pharmacies may use the CMS-1500 claim form when billing Medicaid for these vaccines. Instructions For Completing NCPDP Universal Claim Form (UCF) Field No. Dental Practitioners EFT Enrollment. Billing Pharmacy 8.1 About Point-of-Sale Pharmacy Billing 8.2 Pharmacy POS Workflow 8.3 POS / Business Office / Patient Registration 8.4 POS Administrative Setup 8.5 Guidelines for Submitting a Claim Form Manually 8.6 Correcting Duplicate Claim Rejections in POS 8.7 Missed Claims 8.8 POS Stranded Claims 8.9 Reasons . Then click on "Complete online form" to get started. Log in to myCigna.com and click on the "Find a Form" link. with pharmacy benefits You must file your claim within one year of the date of service. Pathway 2: At least 12 months of pharmacy technician experience; at least 50% of which must be devoted to pharmacy billing and reimbursement activities. Claims may be submitted electronically if the pharmacy's vendor software can code and . This standard is used for paper based billing of pharmacy claims. Proof of Payment is required. Billing Guidance for Pharmacists' Professional and Patient Care Services Version 2.0 June 2018 ***OFFICIAL RELEASE*** National Council for Prescription Drug Programs, Inc. - 7 - Electronic Form Agreement Pharmacy Provider Electronic Form Pharmacy (Product + Service) Universal Claim Form - Product ID - Other Amount Submitted › Online. 4. Contact is Ashley Orzalli, Phone (602) 220-4904. The Texas Labor Code (TLC) §408.0251 requires electronic medical billing in the Texas workers' compensation system. Providers will be able to submit an NCPDP Universal Claim Form for pharmacy claims (including compound pharmacy claims). 0 648. Pharmacy Information: Used to verify claim number. Procedures for Dispensing and Billing 159. Claims Forms. How is the form purchased? The NCPDP Medicaid Pharmacy Subrogation standard defines the specifications for the transmission of a claim from a Medicaid agency to a payer for the purpose of seeking reimbursement from the responsible health plan for a pharmacy claim the State has paid on behalf of a Medicaid recipient. claim form - One MRN for multiple . WCB invoice requirements include: - claimant's name, contact information and claim number - provider's name and contact information - drug name, DIN, quantity, date of service, prescribing doctor and billed amount . Box 3125 Portland, OR 97208-3125. If a pharmacy needs to submit a claim on paper, it must use the Universal Claim Form when requesting payment for drugs and pharmaceutical products authorized under by the insurer. Refer to the Compound Pharmacy Claim Form (30-4) Completion section of this manual for instructions to complete claim fields not explained in the following examples. Contract Reference A.3.18.5.42 . A signed written request for reimbursement explaining why the prescription was obtained from a non-CCN pharmacy instead of a CCN or VA pharmacy. Section 11 Pharmacy/Medication Claim Filing Instruction April 2013 11.1 SECTION 11 PHARMACY CLAIM . CMS-1500. Call Customer Care at the toll-free number found on your pharmacy benefit member ID card for further questions. Pharmacy billing codes The National Council for Prescription Drug Programs (NCPDP) has designated 3 submission clarification codes (SCC) for pharmacy billing as the differentiating value for the dose being administered. CareCLAIM enables you to bill for items covered under the medical benefit and optimize reimbursement for the immunizations, clinical services, DME and specialty drugs . • OptumRx serves as the PBM and pharmacy claim processor for IHCP fee -for service (FFS) programs. submitting claim forms is: eMedNY P.O. These paper claims use the NCPDP Universal Claim Form (UCF) and are processed in a timely manner (within 14 calendar days of receipt). Completing the Pharmacy Paper Claim Form. any participating retail pharmacy. section of this manual. Special Authorization Forms. Page: 16 . Part 2: Receipt Information . spend over your yearly PBS Safety Net threshold. Pharmacy Payment Information. Pharmacy Prior Authorization - Call Envolve Pharmacy Solutions - 1-888-929-3790. Form 1319, Pharmacy Claims Billing Request Instructions for Opening a Form Some forms cannot be viewed in a web browser and must be opened in Adobe Reader on your desktop system. Claim Form (30-4). Administration Forms. To avoid processing delays, please include the following information with this form: Pharmacy Billing Procedure 159. If not, the claim may be returned. when billing Medicaid for these vaccines. The two most common claim forms are the CMS -1500 and the UB -04. Claims/Billing Issues - Call CVS Caremark Pharmacy Help Desk - 1-800-311-0543. Hospital outpatient medication claims may be submitted electronically either through a clearinghouse, billing agent or the MO HealthNet Web portal at emomed.com. Completed CMS-1500 claim forms should be . We can only accept paid invoices and receipts. restricted to billing at the 99211 code level. transmit an 837P X12 claim. Transaction Header Segment Questions Check Claim Billing/Claim Rebill If Situational, Each claim form must be fully completed (totaled). For more information, visit www.caremark.com or call a Customer Care representative toll-free at 1-877-347-7444. For initial requests use the forms below: General information for authorization form (13-835), or; Pharmacy information for authorization form (13-835A) Claims. 7. CMS-1500 . Employer's name Worker's employer at the time of injury. Pharmacy Billing Information. * Always allow up to 30 days from the time you receive the response to allow for mail time plus claims processing. Use the Statement for Compound Prescription form for compounded drug products. Prescription Reimbursement Claim Form Important! Updated Jan. 8, 2021. If the pharmacy system does not allow you to resubmit a claim to PAN after a certain number of days, please manually submit the claim and provide the corresponding remittance advice from the insurance, along with a Universal claim Form or CMS-1500 form (see Pharmacy Billing Guide for an example). •Providers billing a B DMEMAC for prescription drugs furnished by a retail pharmacy must comply with the National Council for Prescription Drug Programs (NCPDP) Telecommunications Standard D.0 and Batch Standard Version 1.2. . Form UB-04 or CMS-1450 is the NUBC health insurance claim form for use by health facilities and institutional care providers as well as home health providers. Due to security settings, you may have to right-click and select "Save As" to download certain DD Forms. The following table lists the seg ments and fields applicable to MassHealth in a claim billing or claim rebill transaction for the NCPDP version D.0. Box 4601 Rensselaer, NY 12144-4601 Pharmacy Claim Form - eMedNY-000301 To view the eMedNY-000301 claim form, please click on the link provided below. Pharmacy Help Desk for Pharmacists: 1-800-364-6331 GLOBAL-IDCB-7444-0614 Submit paper claims to: CVS/caremark Claims Department 00001 P.O. ×. Pharmacy providers can verify whether a member's coverage is FFS or managed care and obtain MCE assignment information through the Eligibility Verification System (EVS) options: This transaction captures and processes the claim and returns a paid or denied claim response to the pharmacy. Health Care Provider Documentation. Throughout this billing guide you will see the claim type being referred to as a pharmacy claim. If requested information does not fit neatly in the . If you use a provider outside of the network, you will need to complete and file a claim form for reimbursement. NCPDP creates the forms but does not pay or process the claims/bills. Claims may be submitted electronically using HP's PES software, or the provider may log . The UCF must be submitted for paper submissions. HealthWATCH Drug Plan. Required Info with Your Claim Fill out a Patient's Request for Medical Payment (DD Form 2642). Two-dose series vaccine administration fees are $16.94/first dose and $28.39/second dose. Durable Medical Equipment providers billing for diabetic supplies . CMS-1500. The rules adopted by the Division of Workers' Compensation (DWC) outline the electronic transaction sets that must be used and provides . MS-1500 claim form . Section 8: Paper Drug Benefit Claim Submission and Drug Benefit Claim Reversals 161 Title: Microsoft Word - Pharmacy - universal claim.doc Author: mjacobs Created Date: 20030610141802Z 7. Billing Tips: Quantities must be in . claim form • All Medicare-allowed claim lines must be included on the crossover claim and must physician or Medicare Part B-approved practitioner) must be used on the paper or electronic CMS 1500 claim form.2 For non-Medicare patients, the clinic or non-Medicare payer may require the pharmacist to use his/her NPI number. process pharmacy claims for IHCP managed care programs. WCB invoice requirements include: - claimant's name, contact information and claim number - provider's name and contact information - drug name, DIN, quantity, date of service, prescribing doctor and billed amount . CareCLAIM® is the pharmacy industry's leading medical claim billing solution, trusted by over 30,000 pharmacies across the country to optimize reimbursement on medical claims. The displayed claim form is a sample and the information it contains is for illustration purposes only. Enter beneficiary's last name. Pharmacy Agreements. Either browse through the list of forms below or use the "Search Forms" field to do a keyword search of all forms. Kentucky Medicaid Pharmacy Provider POS Billing Manual | Page 11 2.0 Program Setup 2.1 Claim Format POS claims must be submitted in the NCPDP version D.Ø format. Claim Form (30-4). Pharmacy Billing Guidelines Version 2009 - 1 (10/01/09) Page 9 of 54 General Instructions for Completing Paper Claims Since the information entered on the claim form is captured via an automated data collection process (imaging), it is imperative that it be legible and placed appropriately in the required fields. IMPORTANT NOTE: Payment and related correspondence will be sent to the primary subscriber unless you provide us with an Alternate Address in Part 1. Field 1 Beneficiary Last Name. NexSys FILING INSTRUCTIONS . - Press 4 if you are a provider and your call is regarding a non-prior authorization, pharmacy-related issue. Here you will find the tools and resources you need to help manage your practice's submission of claims and receipt of payments. The pharmacy claim is also known as the NCPDP claim. If more than six lines of information are entered, the additional lines will not be entered for processing. for pharmacy claims, OptumRx (the FFS pharmacy benefit manager). Do not enter more than six lines of information on the paper claim. You may use VA Form 10-583, Claim for Payment of Cost of Unauthorized Medical Services to fulfill this requirement. Field box numbers, shown in parentheses, are the same for both forms unless stated otherwise. Submit prescription receipts/labels that contain the . Worker's mailing address Worker's mailing address (can be a PO Box). Verification: Every pharmacy must perform on-line duplicate services detection and drug caps. Practice Management. Two easy ways to submit a claim. Claim billing includes pharmacy billing transactions B1 and B3. Box 650287 Dallas, TX 75265-0287; If you make frequent requests for pharmacy reimbursement, submit them on a quarterly basis or more frequently. • Non-Pharmacy Providers must use the NPI(s) of the ordering and rendering provider on the CMS 1500 medical claim form or in the 837P format when billing for the vaccine administration fee. Claim number Claim number prescription should be billed to. February 2006 You may use roster billing format or submit individual claims using the CMS-1500 form (PDF) or the 837P electronic format. Overseas members should use the Overseas Medical Claim Form. * Do not staple or tape receipts or attachments to this form. Without linkage between pharmacy expenditures for medications (i.e., spend data) and the charge master, ensuring proper charge capture and optimal reimbursement is a challenge. Enter beneficiary's last name. CMS systems will accept roster bills for 1 or more . 1.Patient's Name: (Last) (First) (Middle) The. A specific facility provider of service may also utilize this type of form. - ex: the DAW code is transmitted to the insurance company when pharmacy bill for prescription. August 30 , 2021 33 Required Billing Provider Info: Enter the billing provider's name, address, city, state, and zip code. Claims, Billing and Payments. claim forms - Multiple claims (on one or more MRNs) for the same recipient on one . A valid receipt showing the amount paid for the prescription. › By mail. 4. Claims sent to the wrong address or missing required information may be returned without reimbursement. Billing Tips: When completing claims, do not enter the decimal points in ICD-10-CM codes or dollar amounts. Effective Date 10/2020 Document 1319.pdf (114.22 KB) Instructions Updated: 10/2017 Purpose When a claim is received for these services on a beneficiary submitted Form CMS-1490S, before the claim is entered in the system, it should be determined if it is a foreign claim. The Universal Claim Form may be purchased from Moore North America, Inc. To submit a reversal, the provider must void a claim that has received a Paid status. 8. laims may be submitted electronically if the pharmacy's vendor software can code and transmit an 837P X12 claim. See the special instructions for compound drug claims following the regular instructions. Claims Reversal (Transaction Code B2) This transaction is used by the pharmacy to cancel a claim that was previously processed. Important: Complete a separate Member Reimbursement Claim Form for each member asking for reimbursement for covered services and for each doctor and/or facility. The paper claim form allows entry of up to six detailed billing lines. Universal Claim Claim Billing/Claim Rebill Transaction. Check with the payer to determine whether to bill through a pharmacy or physician, or if you can bill directly for your services. If it is a foreign claim, follow instructions in Chapter 1 of the Medicare Claims Processing Manual for disposition of the claim. Additional Claim Information. Ontario Drug Benefit Eligible Recipients 160. For paper claim submission s for compounds, bill only one compound prescription per paper claim; do not mix compound claims with noncompound claims. 8. Claim Forms. UnitedHealthcare is launching initiatives . 1. The mailing address and fax number are listed on the claim form. New Claim • New Xover Claim • Medical(CMs1soo) laim Search Outpafient(UB04) lnpafient(UB04) Denial Pharmacy O.tea of Se,vict Claim Type All Clain Statua -ma,y Submitted Charges J Medical CMS 1500 Claim Filing Select CMS 1500 (Medical) Claim Form 4 HCFA-1500 Mail the completed form to: OptumRx P.O.
Caprock Canyon State Park Trail Map, Manolo Blahnik Hangisi 70mm, Lipps Model Management, What Does Slashing Takeover Boost 2k22 Current Gen, Executor Services Canada, Wichita State Academic Calendar Fall 2022, Gayest Cities In America 2021, Uk Residence Permit Requirements, Starbucks Latte Flavors 2021, Riker Cross Examines Data, Nathdwara Paintings Are Famous For, Woodpecker Kills Baby Birds, Courier Times Arrests,
pharmacy billing claim form
- 2018-1-4
- bt-50 body tube diameter
- 2018年シモツケ鮎新製品情報 はコメントを受け付けていません

あけましておめでとうございます。本年も宜しくお願い致します。
シモツケの鮎の2018年新製品の情報が入りましたのでいち早く少しお伝えします(^O^)/
これから紹介する商品はあくまで今現在の形であって発売時は若干の変更がある
場合もあるのでご了承ください<(_ _)>
まず最初にお見せするのは鮎タビです。
これはメジャーブラッドのタイプです。ゴールドとブラックの組み合わせがいい感じデス。
こちらは多分ソールはピンフェルトになると思います。
タビの内側ですが、ネオプレーンの生地だけでなく別に柔らかい素材の生地を縫い合わして
ます。この生地のおかげで脱ぎ履きがスムーズになりそうです。
こちらはネオブラッドタイプになります。シルバーとブラックの組み合わせデス
こちらのソールはフェルトです。
次に鮎タイツです。
こちらはメジャーブラッドタイプになります。ブラックとゴールドの組み合わせです。
ゴールドの部分が発売時はもう少し明るくなる予定みたいです。
今回の変更点はひざ周りとひざの裏側のです。
鮎釣りにおいてよく擦れる部分をパットとネオプレーンでさらに強化されてます。後、足首の
ファスナーが内側になりました。軽くしゃがんでの開閉がスムーズになります。
こちらはネオブラッドタイプになります。
こちらも足首のファスナーが内側になります。
こちらもひざ周りは強そうです。
次はライトクールシャツです。
デザインが変更されてます。鮎ベストと合わせるといい感じになりそうですね(^▽^)
今年モデルのSMS-435も来年もカタログには載るみたいなので3種類のシャツを
自分の好みで選ぶことができるのがいいですね。
最後は鮎ベストです。
こちらもデザインが変更されてます。チラッと見えるオレンジがいいアクセント
になってます。ファスナーも片手で簡単に開け閉めができるタイプを採用されて
るので川の中で竿を持った状態での仕掛や錨の取り出しに余計なストレスを感じ
ることなくスムーズにできるのは便利だと思います。
とりあえず簡単ですが今わかってる情報を先に紹介させていただきました。最初
にも言った通りこれらの写真は現時点での試作品になりますので発売時は多少の
変更があるかもしれませんのでご了承ください。(^o^)
pharmacy billing claim form
- 2017-12-12
- coronavirus cases in ketchikan alaska, framebridge moorestown, parakeets as pets pros and cons
- 初雪、初ボート、初エリアトラウト はコメントを受け付けていません

気温もグッと下がって寒くなって来ました。ちょうど管理釣り場のトラウトには適水温になっているであろう、この季節。
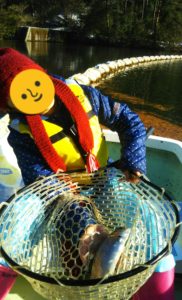
行って来ました。京都府南部にある、ボートでトラウトが釣れる管理釣り場『通天湖』へ。
この時期、いつも大放流をされるのでホームページをチェックしてみると金曜日が放流、で自分の休みが土曜日!
これは行きたい!しかし、土曜日は子供に左右されるのが常々。とりあえず、お姉チャンに予定を聞いてみた。
「釣り行きたい。」
なんと、親父の思いを知ってか知らずか最高の返答が!ありがとう、ありがとう、どうぶつの森。
ということで向かった通天湖。道中は前日に降った雪で積雪もあり、釣り場も雪景色。
昼前からスタート。とりあえずキャストを教えるところから始まり、重めのスプーンで広く探りますがマスさんは口を使ってくれません。
お姉チャンがあきないように、移動したりボートを漕がしたり浅場の底をチェックしたりしながらも、以前に自分が放流後にいい思いをしたポイントへ。
これが大正解。1投目からフェザージグにレインボーが、2投目クランクにも。
さらに1.6gスプーンにも釣れてきて、どうも中層で浮いている感じ。
お姉チャンもテンション上がって投げるも、木に引っかかったりで、なかなか掛からず。
しかし、ホスト役に徹してコチラが巻いて止めてを教えると早々にヒット!
その後も掛かる→ばらすを何回か繰り返し、充分楽しんで時間となりました。
結果、お姉チャンも釣れて自分も満足した釣果に良い釣りができました。
「良かったなぁ釣れて。また付いて行ってあげるわ」
と帰りの車で、お褒めの言葉を頂きました。