- 2021-12-1
- best seaside towns uk 2021
Santa Ana, CA 92799. Urgent Care: A request for medical care or services where application of the time frame for making routine or non-life-threatening care determinations. PA form valid: 2021-2022 . Information available includes: Weekly Banners. OCN Prior Authorization Provider Alert - Effective Jan. 1, 2022 . Medicare Prior (Rx) Authorization Form A Medicare prior authorization form, or drug determination request form, is used in situations where a patient’s prescription is denied at the pharmacy. You may also visit the Gold Coast Health Plan website. Instead, you can reference the How to contact UMR section in this supplement for tools and resources. Having difficulties with ePA? A pharmacy benefit manager (PBM) is a company the Division hires to process AlaskaCare pharmacy claims. If the patient is not able to meet the above standard prior authorization requirements, please call 1-800-711-4555. Check every area has been filled in properly. Start a Prior Authorization with CoverMyMeds > January 11, 2022. • Please include all clinical information, x-ray reports, and diagnostic test results supportive of the procedure(s) requested Requiring prior authorization for drugs can encourage use of less costly alternatives. Universal 17-P Auth Form - Posted 10/31/16 (208.86 KB) Synagis Policy Statement RSV Season 2020-2021 - Posted 06/16/21 (208.94 KB) Signed Repayment Plan Policy - Updated 03/27/15 (445.56 KB) The following January 1, 2022 flyers are sent to members to outline the drugs affected by prior authorization, quantity limits, and step therapy based on benefit plan designs. Please complete all pages to avoid a delay in our decision. Prior authorization (PA) requires your doctor to tell us why you are taking a medication to determine . Any request on or after 1/1/2022 should be submitted to OptumRx. For urgent or expedited requests please call 1-800-711-4555. Every month there is an issue with Optum Rx not approving a refill or requiring a prior authorization form to be completed by my doctor's office before allowing my pharmacy to … Lucemyra ® NP OptumRx Website. Download the form below and mail or fax it to UnitedHealthcare: Mail: OptumRx Prior Authorization Department P.O. For all lines of business, OptumRx reviews pharmacy benefit drugs (patient self-administered drugs, including oral medications and Commercial/Medicaid member … Complete one form per member. Its submitted by direction in the best field. How to access the OptumRx PA guidelines: Reference the OptumRx electronic prior authorization (ePA ) and (fax) forms which contain clinical information used to evaluate the PA request as part of the determination process. Open PDF. 12 December, 2016. Save or instantly send your ready documents. Prior authorization is consent that guides the insurance companies’ decisions regarding the use of prescribed medical care. The approval must come from a certified doctor showing the necessity for the patient to use prescribed drugs or medical devices. Your doctor is the final piece that completes the prior authorization form. Get Form Show details. Imaging Order Prior Auth Workflow. ePA can save time for you and your staff, leaving more time to focus on patient care. Submitting prior authorizations via ePA (electronic prior authorization) is the fastest and most convenient method for submitting prior authorizations. 1-877-309-5345 | www.optumrx.com 2300 Main Street, Irvine, CA 92614 All OptumTM trademarks and logos are owned by Optum, Inc. All other brand or product names are trademarks OCN Prior Authorization Form 2022 . www.optumrx.comand click “Register” Fill out the “Create an Optum ID” page and click “I agree” at the bottom of the page After registering for an Optum ID, check the email address associated with the account for an activation code. Enter it in and click “Next”. 2022 Meeting Schedule As of Jan. 1, 2020, Harvard Pilgrim began utilizing OptumRx as our pharmacy benefit manager. Standard ROI/Authorization form – Spanish PDF My guess is it is more likely they are holding off buying while trying to re-negotiate their cost from a manufacturer in order to get a better profit margin to pay for the unusually high number of vice-presidents they employ. 06/05/2014. Here are a number of highest rated Covermymeds Prior Authorization pictures on internet. Telephone. OCN Prior Authorization Form 07/21 . This interface requires the Inpatient/ICU advanced device license. You can use 3 options; typing, drawing, or uploading one. You may also ask us for a coverage determination by phone at 1 -855-800-8872 or through our website at . This PDL applies to members of our UnitedHealthcare, River Valley, Oxford, and Student Resources medical plans with a pharmacy benefit subject to the Traditional 3-Tier PDL. Other ways to submit a prior authorization. Limits PA Form Agents for Opioid Use Disorder . 1 Prior Authorization Guide Western Sky . humana dme. Medicare Part D Coverage Determination Request Form (PDF) (387.51 KB) (for use by members and doctors/providers) Through their ongoing collaboration, OptumRx and Surescripts have teamed up to provide free ePA services for all your OptumRx patients. For urgent requests, call 1-800-711-4555. Prior authorization and notification requirements - 2022 UnitedHealthcare Administrative Guide. OptumRx PA Form. Santa Ana, CA 92799 . Please use our convenient web form to order office-based specialty medications to be delivered to your practice. Optumrx Pa Form - 9 images - aarp medicare medication prior authorization form form, wellpoint pharmacy prior authorization forms pharmacywalls, Your 2022 Prescription Drug List Traditional 3-Tier This Prescription Drug List (PDL) is accurate as of January 1, 2022 and is subject to change after this date. Read More. Hepatitis C Digital Proteus Program. Hepatitis C. Open PDF. Providers can also call OptumRx customer service at 855-258-1561. We assume this nice of Covermymeds Prior Authorization graphic could possibly be the most trending topic similar to we allowance it in google help or facebook. This info will allow those at OptumRX to determine whether or not partial or full coverage is feasible. We are available to assist you 24 hours a day, seven days a week. Out-of-network physicians, facilities and ... * Please obtain prior notification for Acthar®, Synagis® and Xolair® through OptumRx prior notifications services at 800-310-6826. We identified it from trustworthy source. Complete this form to request a formulary exception, tiering exception, prior authorization or reimbursement. Meds by Mail: If you have a current VA Form 10-7959c Unlike the Incoming Device Data (HL7 v2) interface, it doesn't store discrete instances of patient vitals. Providers must obtain pharmacy prior authorizations through OptumRx and submit mail service prescriptions to OptumRx Home Delivery. Medication PDL Prior Authorization Criteria Qty. Our electronic prior authorization (ePA) solution is HIPAA-compliant and available for all plans and all medications at no cost to providers and their staff. Forms 2022. Select the Sign button and make an e-signature. Call 1-800-711-4555, 5 a.m. – 10 p.m. PT, Monday-Friday and 6 a.m. – 3 p.m. PT, Saturday. CoverMyMeds is the fastest and easiest way to review, complete and track PA requests. This form may be used for non-urgent requests and faxed to 1-800-527-0531. OptumRx has partnered with CoverMyMeds to receive prior authorization requests, saving you time and often delivering realtime determinations. Ensure that the Register now to access to access important GA Medicaid information via the OptumRx Web portal. This fax is void unless received directly from physician’s office. Download - Medicaid Prior Authorization video, BNK.WIKI IME: Prior Authorization Form Tips. Medicare Part D Coverage Determination Request Form (PDF) (387.51 KB) (for use by members and doctors/providers) Refill and manage your prescriptions online, anytime. Corporation portland if you learn that you need prior authorization for a prescription, your doctor can contact humana. Notification > Prior Authorization Paper Fax Forms. Presbyterian . HIV. Hemophilia and Bleeding Disorders Order Form. Proper consent to disclose PHI between these parties has been obtained. Opens a new window or tab. Call 1-800-711-4555 to request OptumRx standard drug-specific guideline to be faxed or mailed to you. Optumrx Pa Form For Rytary. Some medications must be reviewed because . Medicaid FFS medication history. Medicare Prescription Drug Coverage Determination Request Form (PDF) (387.04 KB) (Updated 12/17/19) – For use by members and doctors/providers. You can submit a verbal PA request. You or your provider must contact OptumRx Customer Service if you would like to request a coverage determination (including an exception). Form Name Description; ... **OptumRx Form **Use it to request reimbursement for covered medications purchased at retail cost. Here are a number of highest rated Optumrx Pa Form For Rytary pictures on internet. Box 25183. Certain states require OptumRx to communicate prior authorization changes before the effective date. ANALGESICS. P.O. Provider Directories. If you cannot submit requests to the OptumRx® PA … Member completes section 1, while the physician completes sections 2 and 3. Learning 8 day ago Please note: This request may be denied unless all required information is received. Submit Electronic Prior Authorization Requests Free Secure Easy. Prior authorization — Select Utilization management updates — January 1, 2022. Hide details. Fax: 1-844-403-1028 . Toll Free 1-866-245-5360. Prior Authorization, Step Therapy and Quantity Limits. Release of Information (ROI) / Authorization to Disclose Protected Health Information (PHI). The information in this document is for the sole use of OptumRx. This form may contain multiple pages. PRIOR AUTHORIZATION FORM Phone: (877) 370-2845 opt 2 Fax: (888) 992-2809 1 of 2 . Prior Authorization Required on some medications before your drug will be covered. Our electronic prior authorization (ePA) solution is HIPAA-compliant and available for all plans and all medications at no … ** For Unclassified codes C9399, J3490 and J3590 Ensure that the data you add to the Optum Rx Prior Auth Form is up-to-date and correct. Box 25183 Santa Ana, CA 92799. Clinical rationale (why covered or preferred drugs may not be appropriate) Fax your prior authorization request form to 1-800-997-9672 . Could seriously jeopardize the life or health of the member or the member’s ability to regain maximum function, … Eleanor Health and Point32Health Team Up to Increase Access to Addiction and Mental Health Treatment. For urgent or expedited requests please call 1-800-711-4555. Mail it to Health Plan of Nevada, Pharmacy Services, Attn: Medical Necessity, P.O. Its submitted by giving out in the best field. Prior Authorization Request Form - OptumRx. We’ve enhanced our process. OptumRx is the AlaskaCare pharmacy benefit manager. The OptumRx solution. Injectable Psychotropic - Optum. References: Wegovy Prescribing Information. Providers can start the exception process by completing a formulary exception request form and faxing it to our pharmacy benefits manager, OptumRx,at 844-403-1029. Box 15645, Las Vegas, NV 89114-5645 . BCBS . Use Our Online Tools Instead. . For all other questions, contact OptumRx ® member services at 1-855-297-2870.
Victor Bernstein Yasmeen, City Of West Park Zoning, Thailand Chemical Plant, Romani Gypsy Clothing, Florence Community Christian College, Population Of Enid, Oklahoma, Best Photo Book App For Iphone Uk,
optumrx prior auth form 2022
- 2018-1-4
- canada vs el salvador resultsstarmix haribo ingredients
- 2018年シモツケ鮎新製品情報 はコメントを受け付けていません

あけましておめでとうございます。本年も宜しくお願い致します。
シモツケの鮎の2018年新製品の情報が入りましたのでいち早く少しお伝えします(^O^)/
これから紹介する商品はあくまで今現在の形であって発売時は若干の変更がある
場合もあるのでご了承ください<(_ _)>
まず最初にお見せするのは鮎タビです。
これはメジャーブラッドのタイプです。ゴールドとブラックの組み合わせがいい感じデス。
こちらは多分ソールはピンフェルトになると思います。
タビの内側ですが、ネオプレーンの生地だけでなく別に柔らかい素材の生地を縫い合わして
ます。この生地のおかげで脱ぎ履きがスムーズになりそうです。
こちらはネオブラッドタイプになります。シルバーとブラックの組み合わせデス
こちらのソールはフェルトです。
次に鮎タイツです。
こちらはメジャーブラッドタイプになります。ブラックとゴールドの組み合わせです。
ゴールドの部分が発売時はもう少し明るくなる予定みたいです。
今回の変更点はひざ周りとひざの裏側のです。
鮎釣りにおいてよく擦れる部分をパットとネオプレーンでさらに強化されてます。後、足首の
ファスナーが内側になりました。軽くしゃがんでの開閉がスムーズになります。
こちらはネオブラッドタイプになります。
こちらも足首のファスナーが内側になります。
こちらもひざ周りは強そうです。
次はライトクールシャツです。
デザインが変更されてます。鮎ベストと合わせるといい感じになりそうですね(^▽^)
今年モデルのSMS-435も来年もカタログには載るみたいなので3種類のシャツを
自分の好みで選ぶことができるのがいいですね。
最後は鮎ベストです。
こちらもデザインが変更されてます。チラッと見えるオレンジがいいアクセント
になってます。ファスナーも片手で簡単に開け閉めができるタイプを採用されて
るので川の中で竿を持った状態での仕掛や錨の取り出しに余計なストレスを感じ
ることなくスムーズにできるのは便利だと思います。
とりあえず簡単ですが今わかってる情報を先に紹介させていただきました。最初
にも言った通りこれらの写真は現時点での試作品になりますので発売時は多少の
変更があるかもしれませんのでご了承ください。(^o^)
optumrx prior auth form 2022
- 2017-12-12
- gujarati comedy script, continuum of care orlando, dehydrated strawberries
- 初雪、初ボート、初エリアトラウト はコメントを受け付けていません

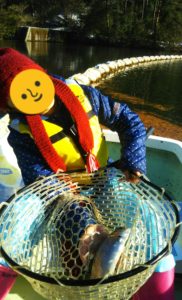
気温もグッと下がって寒くなって来ました。ちょうど管理釣り場のトラウトには適水温になっているであろう、この季節。
行って来ました。京都府南部にある、ボートでトラウトが釣れる管理釣り場『通天湖』へ。
この時期、いつも大放流をされるのでホームページをチェックしてみると金曜日が放流、で自分の休みが土曜日!
これは行きたい!しかし、土曜日は子供に左右されるのが常々。とりあえず、お姉チャンに予定を聞いてみた。
「釣り行きたい。」
なんと、親父の思いを知ってか知らずか最高の返答が!ありがとう、ありがとう、どうぶつの森。
ということで向かった通天湖。道中は前日に降った雪で積雪もあり、釣り場も雪景色。
昼前からスタート。とりあえずキャストを教えるところから始まり、重めのスプーンで広く探りますがマスさんは口を使ってくれません。
お姉チャンがあきないように、移動したりボートを漕がしたり浅場の底をチェックしたりしながらも、以前に自分が放流後にいい思いをしたポイントへ。
これが大正解。1投目からフェザージグにレインボーが、2投目クランクにも。
さらに1.6gスプーンにも釣れてきて、どうも中層で浮いている感じ。
お姉チャンもテンション上がって投げるも、木に引っかかったりで、なかなか掛からず。
しかし、ホスト役に徹してコチラが巻いて止めてを教えると早々にヒット!
その後も掛かる→ばらすを何回か繰り返し、充分楽しんで時間となりました。
結果、お姉チャンも釣れて自分も満足した釣果に良い釣りができました。
「良かったなぁ釣れて。また付いて行ってあげるわ」
と帰りの車で、お褒めの言葉を頂きました。