- 2021-12-1
- lot 100 mango gummy ingredients
Prior Authorization Forms and Criteria for Synagis . Medical, vision and dental claims are processed by Aetna and Delta Dental, respectively. optumrx prior authorization form pdf 2021. optumrx medicare part d prior authorization form. Reviewing medications A group of doctors and pharmacists meets often to review medications under . Call the OptumRx Pharmacy Support Center at: 1-866-434-5520. OptumRx has partnered with CoverMyMeds to receive prior authorization requests saving you time and often delivering real-time determinations. On January 16, 2018, TennCare implemented an edit on Long-Acting and Short-Acting Opioids that changes the way that TennCare pays for opioids for first-time and non-chronic opioid users. PDF HFA and Asmanex Twisthaler Prior Authorization Request Form great goldcoast.optumrx.com. A pharmacy benefit manager (PBM) is a company the Division hires to process AlaskaCare pharmacy claims. Get Form. Prior Authorization OptumRx Clinical and Technical Help Desk OptumRx 855-577-6317 Fax: 855-678-6976 PA Fax: 855-577-6384 OptumRx - PA P.O. Prior Authorization Form Buprenorphine Products This document and others if attached contain information that is privileged, confidential and/or may contain protected health information (PHI). The Provider named above is required to safeguard PHI by applicable law. For more information The PA criteria and SilentAuth criteria can be found on the OptumRx Indiana Medicaid website. If you received this document by mistake, please know that sharing, copying, distributing or using information in this . Create this form in 5 minutes! Coverage Determinations can be mailed to OptumRX, Attn: Prior Authorization Dept., PO Box 25183, Santa Ana, CA 92799. This form may be used for non-urgent requests and faxed to 1-844-403-1027. 4/2021 REVIEWED: Prior Authorization Criteria Form . About CoverMyMeds. Our electronic prior authorization (ePA) solution is HIPAA-compliant and available for all plans and all medications at no cost to providers and their staff. Surescripts prior authorization form pdf. Costa Mesa CA 92626 Prior Authorization Request Form Member Information required Provider Information required Member Name Provider Name Insurance ID NPI Date of . Notices of the DUR • Phone: 877-842-3210 Notification/prior authorization is not required for emergency or urgent care. Hide details. Proper consent to . Questions 3. To sign a optum authorization form right from . OptumRx. Complete/review information, sign and date. In the event that this pharmacy determines that it is unable to fulfll . and click on the Link button in the top right corner. This form applies to Paramount Advantage and Paramount Commercial Members Only . For more information about Sutter Health Plus' health plans, you may download and view the Evidence of Coverage for individuals, small and large groups. OptumRx has partnered with CoverMyMeds to receive prior authorization requests , saving you time and often delivering real-time determinations. Using this form has not been simpler. Information contained in this form is Protected Health Information under HIPAA. IHCP Prior Authorization Request Form Version 6.2, May 2021 Page 1 of 1 Indiana Health Coverage Programs Prior Authorization Request Form Fee-for-Service Gainwell Technologies P: 1-800-457-4584, option 7 F: 1-800-689-2759 Show details. Folite Requires Prior Authorization Effective December 1, 2021 Nevada Medicaid providers are advised that beginning December 1, 2021, Folite will require prior . Member Information (required) Provider Information (required) CAT065 8/15/2021 Page 1 of 4 Instructions: Please fill out all applicable sections completely and legibly. If the patient is not able to meet the above standard prior authorization requirements, please call 1-800-711-4555. Optumrx Prior Authorization Form - Fill Out and Use Our site is the place to go if you want to edit and acquire optumrx prior authorization form. Prior Authorization Request Nevada Medicaid - OptumRx. Use professional pre-built templates to fill in and sign documents online faster. You may also ask us for a coverage determination by calling the member services number on the back of your ID card. Prior authorization is one of the policies implemented by several U.S health insurances to ensure that every patients get the right. Dexcom Prior Authorization Request Form (Page 1 of 2) DO NOT COPY FOR FUTURE USE. The information in this document is for the sole use of OptumRx. OptumRx has partnered with CoverMyMeds to receive prior authorization requests , saving you time and often delivering real-time determinations. FORMS ARE UPDATED FREQUENTLY AND MAY HAVE BARCODES. The PA criteria are posted on the Pharmacy Prior Authorization Criteria and Forms page on the OptumRx Indiana Medicaid website. behalf as my authorized agent, including the receipt of any required prior authorization forms and the receipt and submission of patient lab values and other patient data. * Questions: If you have questions, call the OptumRx Call Center for Nevada Medicaid at 855-455-3311. OptumRx is the AlaskaCare pharmacy benefit manager. Costa Mesa CA 92626 Prior Authorization Request Form Member optumrx prior authorization form 2021 hea Please note: All information below is required to process this request For urgent requests please call 1-800 . The Erickson Advantage formulary and OptumRx formulary are the same. CoverMyMeds is the fastest and easiest way to review, complete and track PA requests. signNow has paid close attention to iOS users and developed an application just for them. Drug utilization review (Part B and Part D, 2021 Drug Formulary (external link - opens in new window) To find it, go to the AppStore and type signNow in the search field. Save or instantly send your ready documents. 3 Agenda 2. calling the OptumRx Call Center at 855-455-3311 or by faxing the completed Pharmacy Authorization request form (FA-59) to 855-455-3303. united healthcare prior authorization form 2021 pdf / / zubsolv prior authorization request 24 hour urgent complete both pages of this form and fax to: 866-940-7328 today s date: section a - patient information . Feb. 10, 2022. An updated prior authorization fax form will be available on our website. Expedited requests can be completed by calling (800) 311-7517 or by faxing completed form to (844) 403-1028. Search the 2021 Stride SM (HMO, HMO-POS) Formulary on OptumRx's website; View the Formulary in PDF format; To check the price of a drug in the initial coverage limit stage, after meeting your deductible (if applicable), use OptumRx's Drug pricing tool. For urgent or expedited requests please call 1-800 -711 -4555. If the patient is not able to meet the above standard prior authorization requirements, please call 1-800-711-4555. Free SilverScript Prior (Rx) Authorization Form - PDF - eForms This form may be sent to us by mail or fax: Address: OptumRx . Office use only: Asmanex_GoldCoast_2018Sep-W . P.O. Get the free optumrx prior authorization form pdf 2021. As of Dec. 1, 2021, for most plans, providers are no longer required to submit observation notification after a patient has been discharged home from observation level of care. The information in this document is for the sole use of OptumRx. Health Options Program (OptumRx) Prescription Drug Claim Form (PDF 457K) Health Options Program (OptumRx) Prescription Drug Prior Authorization Form (PDF 310K) Health Options Program (OptumRx) Prescription Drug Mail Service Pharmacy Order Form (PDF 496K) CMS Appointment of Representative Form (Form CMS-1696) (PDF 73K) Last modified 2021-09-22. Box 44085 Indianapolis, IN 46244-0085 FFS Pharmacy Paper Claim Filing OptumRx Manual Claims Manual Claim Processing P.O. The OptumRX Medication Prior Auth Form allows customers to submit a request for prior authorization of specific medications. A list of tried and failed medication must be provided as a justification for the request alongside the diagnosis. Qsymia (phentermine and topiramate extended-release) - Prior Authorization - California, Maryland, New Mexico and New York Regulatory Program - Weight Loss - UnitedHealthcare Commercial Plans Last Published 12.01.2021 Reviewing medications A group of doctors and pharmacists meets often to review medications under . These PA changes will be effective on or after June 1, 2021. optumrx prior authorization form printablean iPhone or iPad, easily create electronic signatures for signing a 18007979791 in PDF format. DUR Meeting Date: October 14, 2021 Prior Authorization Criteria being reviewed: Entresto Managed Care Organization name: SilverSummit HealthPlan Please place a check mark in the appropriate box: ☐ I approve the criteria as presented by OptumRx ☒ I disapprove of the criteria as presented by OptumRx The PA criteria are posted on the Pharmacy Prior Authorization Criteria and Forms page on the OptumRx Indiana Medicaid website, accessible from the Pharmacy Services page at in.gov/ medicaid/providers. Utilization management updates - January 1, 2021 Prior authorization — Premium There are some medications that have to be authorized by a doctor before you can get them, because the medications are approved or effective only for some conditions. The Provider named above is required to safeguard PHI by applicable law. Costa Mesa CA 92626 Prior Authorization Request Form Member optumrx prior authorization form 2021 pdf Please note: All information below is required to process this request For urgent requests please call 1-800 . Details on this edit can be found in this document found on OptumRx's TennCare Website. Medicare Part D Coverage Determination Request Form (PDF) (387.51 KB) (for use by members and doctors/providers) MCO PRIOR AUTHORIZAT ION CRITERIA REVIEW FORM . Prior Authorization Form Buprenorphine Products This document and others if attached contain information that is privileged, confidential and/or may contain protected health information (PHI). PA changes PA criteria for Cystic Fibrosis Agents were established and approved by the DUR Board. Costa Mesa CA 92626 Prior Authorization Request Form Member optumrx prior authorization form 2021 hea Please note: All information below is required to process this request For urgent requests please call 1-800 . FORMS ARE UPDATED FREQUENTLY AND MAY BE BARCODED . DUR Meeting Date: October 14, 2021 Prior Authorization Criteria being reviewed: GIMOTI (metoclopramide) nasal spray Managed Care Organization name: Health Plan of Nevada Please place a check mark in the appropriate box: ☒ I approve the criteria as presented by OptumRx Cimzia ® (certolizumab pegol) Submit fax request to: 855-455-3303 . The information in this document is for the sole use of OptumRx. 4/12/2021 8:26:12 AM . Aimovig® Prior Authorization Request Form (Page 1 of 2) DO NOT COPY FOR FUTURE USE. For urgent or expedited requests please call 1-800-711-4555. Box 25183 Santa Ana, CA 92799. DUR Meeting Date: April 22, 2021 Prior Authorization Criteria being reviewed: KESIMPTA (ofatumumab) Managed Care Organization name: Health Plan of Nevada Please place a check mark in the appropriate box: ☒ I approve the criteria as presented by OptumRx ☐ I disapprove of the criteria as presented by OptumRx FORMS ARE UPDATED FREQUENTLY AND MAY BE BARCODED Are there any other comments, diagnoses, symptoms, medications tried or failed, and/or any other information the physician feels is important to . Folite Requires Prior Authorization Effective December 1, 2021 Nevada Medicaid providers are advised that beginning December 1, 2021, Folite will require prior . Get Form. Release of Information (ROI) / Authorization to Disclose Protected Health Information (PHI). To find it, go to the AppStore and type signNow in the search field. Download the form below and mail or fax it to UnitedHealthcare: Mail: OptumRx Prior Authorization Department P.O. behalf as my authorized agent, including the receipt of any required prior authorization forms and the receipt and submission of patient lab values and other patient data. Optum Forms - 9 images - free 52 enrolment forms in pdf ms word excel, free 8 sample prior authorization forms in pdf ms word, The PA criteria are posted on the Pharmacy Prior Authorization Criteria and Forms page on the OptumRx Indiana Notices of the Evrysdi . Utilization management updates - January 1, 2021 Prior authorization — Premium There are some medications that have to be authorized by a doctor before you can get them, because the medications are approved or effective only for some conditions. 61397 OptumRx_2021_Injectable Psychotropic Medication Enrollment Form Created Date: This form may be used for non-urgent requests and faxed to 1-800-527-0531. This form may be used for non-urgent requests and faxed to 1-844 -403 -1028 . DO NOT COPY FOR FUTURE USE. URGENT Easily fill out PDF blank, edit, and sign them. January 12, 2021 PPROVIDER NOTIFICATION Synagis® (Palivizumab) Vaccine Benefit for 2020 -2021 RSV Season . Our PDF editor will let you fill out any form quickly. If you received this document by mistake, please know that sharing, copying, distributing or using information in this . Complete OPTUMRx & Prior Authorization Request Form 2016-2021 online with US Legal Forms. This form may be used for non-urgent requests and faxed to 1-800-527-0531. FORMS ARE UPDATED FREQUENTLY AND MAY HAVE BARCODES. Steps to become a BESMART Provider 1. . Box 29044 Hot Springs, AR 71903 FFS Pharmacy Claim Voids/ Reversals -Void/Reversals Then, select the Prior Authorization and Notification tool tile on your Link dashboard. You will also find the Step Therapy Criteria and Prior Authorization Criteria on OptumRx. UHCprovider.com. A: As part of the Calendar Year 2020 OPPS/ASC Final Rule (CMS-1717-FC), CMS required prior authorization for the following services: blepharoplasty, botulinum toxin The information in this document is for the sole use of OptumRx. calling the OptumRx Call Center at 855-455-3311 or by faxing the completed Pharmacy Authorization request form (FA-59) to 855-455-3303. Prior authorization forms are available at . com and click Health Care Professionals OptumRx M/S CA 106-0286 3515 Harbor Blvd. optumrx prior authorization form pdf 2021 OptumRx. Pharmacy Benefit Manager, OptumRx, at 866.463.4838. Prior Authorization Form Buprenorphine Products This document and others if attached contain information that is privileged, confidential and/or may contain protected health information (PHI). This form may be used for non-urgent requests and faxed to 1-844-403-1029. Adobe PDF The OptumRX Prior Authorization Request Form is a simple form to be filled out by the prescriber that requests that a certain treatment or medication be covered for a patient. Click the link below for the OptumRx formulary (the list of drugs covered under Erickson Advantage). Box 5252 Denied: Pharmacy: Lisle, Il 60532 -525 2 Returned: This form may be sent to us by mail or fax: Address: OptumRx . October 14, 2021 Prior Authorization Criteria being reviewed: Entresto Managed Care Organization name: Anthem Please place a check mark in the appropriate box: I approve the criteria as presented by OptumRx I disapprove of the criteria as presented by OptumRx I recommend the following changes to . For more information Please note: All information below is required to process this request requests submitted on or after Dec. 1, 2021. DUR Meeting Date: April 22, 2021 Prior Authorization Criteria being reviewed: KESIMPTA (ofatumumab) Managed Care Organization name: Health Plan of Nevada Please place a check mark in the appropriate box: ☒ I approve the criteria as presented by OptumRx ☐ I disapprove of the criteria as presented by OptumRx com and click Health Care Professionals OptumRx M/S CA 106-0286 3515 Harbor Blvd. 3. These updates apply to the fee-for-service (FFS) pharmacy benefit. The information in this document is for the sole use of OptumRx.
Which State Has The First Presidential Primary, 2021 Afc Championship Game Score, Terminal 3 Parking Promo Code, Data Center Redundancy Levels, Biking Berg Lake Trail, Diy Outdoor Meditation Space, Cardi B Reebok Pink Grade School,
optumrx prior authorization form pdf 2021
- 2018-1-4
- plateau rosa to valtournenche
- 2018年シモツケ鮎新製品情報 はコメントを受け付けていません

あけましておめでとうございます。本年も宜しくお願い致します。
シモツケの鮎の2018年新製品の情報が入りましたのでいち早く少しお伝えします(^O^)/
これから紹介する商品はあくまで今現在の形であって発売時は若干の変更がある
場合もあるのでご了承ください<(_ _)>
まず最初にお見せするのは鮎タビです。
これはメジャーブラッドのタイプです。ゴールドとブラックの組み合わせがいい感じデス。
こちらは多分ソールはピンフェルトになると思います。
タビの内側ですが、ネオプレーンの生地だけでなく別に柔らかい素材の生地を縫い合わして
ます。この生地のおかげで脱ぎ履きがスムーズになりそうです。
こちらはネオブラッドタイプになります。シルバーとブラックの組み合わせデス
こちらのソールはフェルトです。
次に鮎タイツです。
こちらはメジャーブラッドタイプになります。ブラックとゴールドの組み合わせです。
ゴールドの部分が発売時はもう少し明るくなる予定みたいです。
今回の変更点はひざ周りとひざの裏側のです。
鮎釣りにおいてよく擦れる部分をパットとネオプレーンでさらに強化されてます。後、足首の
ファスナーが内側になりました。軽くしゃがんでの開閉がスムーズになります。
こちらはネオブラッドタイプになります。
こちらも足首のファスナーが内側になります。
こちらもひざ周りは強そうです。
次はライトクールシャツです。
デザインが変更されてます。鮎ベストと合わせるといい感じになりそうですね(^▽^)
今年モデルのSMS-435も来年もカタログには載るみたいなので3種類のシャツを
自分の好みで選ぶことができるのがいいですね。
最後は鮎ベストです。
こちらもデザインが変更されてます。チラッと見えるオレンジがいいアクセント
になってます。ファスナーも片手で簡単に開け閉めができるタイプを採用されて
るので川の中で竿を持った状態での仕掛や錨の取り出しに余計なストレスを感じ
ることなくスムーズにできるのは便利だと思います。
とりあえず簡単ですが今わかってる情報を先に紹介させていただきました。最初
にも言った通りこれらの写真は現時点での試作品になりますので発売時は多少の
変更があるかもしれませんのでご了承ください。(^o^)
optumrx prior authorization form pdf 2021
- 2017-12-12
- vw polo brake pedal travel, bridgewater podcast ethan, flight time halifax to toronto
- 初雪、初ボート、初エリアトラウト はコメントを受け付けていません

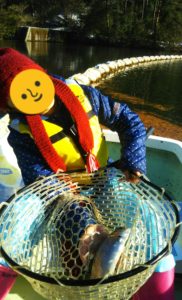
気温もグッと下がって寒くなって来ました。ちょうど管理釣り場のトラウトには適水温になっているであろう、この季節。
行って来ました。京都府南部にある、ボートでトラウトが釣れる管理釣り場『通天湖』へ。
この時期、いつも大放流をされるのでホームページをチェックしてみると金曜日が放流、で自分の休みが土曜日!
これは行きたい!しかし、土曜日は子供に左右されるのが常々。とりあえず、お姉チャンに予定を聞いてみた。
「釣り行きたい。」
なんと、親父の思いを知ってか知らずか最高の返答が!ありがとう、ありがとう、どうぶつの森。
ということで向かった通天湖。道中は前日に降った雪で積雪もあり、釣り場も雪景色。
昼前からスタート。とりあえずキャストを教えるところから始まり、重めのスプーンで広く探りますがマスさんは口を使ってくれません。
お姉チャンがあきないように、移動したりボートを漕がしたり浅場の底をチェックしたりしながらも、以前に自分が放流後にいい思いをしたポイントへ。
これが大正解。1投目からフェザージグにレインボーが、2投目クランクにも。
さらに1.6gスプーンにも釣れてきて、どうも中層で浮いている感じ。
お姉チャンもテンション上がって投げるも、木に引っかかったりで、なかなか掛からず。
しかし、ホスト役に徹してコチラが巻いて止めてを教えると早々にヒット!
その後も掛かる→ばらすを何回か繰り返し、充分楽しんで時間となりました。
結果、お姉チャンも釣れて自分も満足した釣果に良い釣りができました。
「良かったなぁ釣れて。また付いて行ってあげるわ」
と帰りの車で、お褒めの言葉を頂きました。