- 2021-12-1
- lot 100 mango gummy ingredients
Use our testing locator . Medicare ABN Specific Modifiers – GA, GX, GY, GZ. Insurers are already required to cover diagnostic lab COVID-19 testing when ordered by a physician or health care provider. You can Medicare is not covered under the new plan. The Vietnam government is making large strides to achieve 90% Universal Health Coverage (UHC), and aims for 95% by 2025. was established in 2002 which is the investment holding subsidiaries of Grand Pharma (China) Co. VF in accordance with the new regulations that require Health plans to reimburse members for FDA-approved COVID-19 rapid antigen tests. Mid-Missourians with private health insurance are now able to get up to eight free at-home COVID-19 test kits per month. This test requires spitting into a collection tube so it may not be appropriate for young children *** If you are planning to travel, saliva specimen tests are often not acceptable for travel. Posted 1/7/2022. If it is appropriate for you to receive a COVID-19 diagnostic test, we will cover FDA-authorized tests. Members Stay informed about coronavirus (COVID-19) Providers Stay informed about coronavirus (COVID-19) Browse our Mental Health Providers: Browse our Medical and Administrative policies: Information for NY SHOP In order to maximize your reimbursement, you should buy SINGLE TEST KITS ONLY. People with Medicare can access one free lab-performed test per year without an order. AAFP says Z11.52 should be used when patients being screened for COVID-19 have no symptoms, no known exposure to the virus, and test results that are either unknown or negative. With yet another testing code, you may be a little confused as to which code to use for what test. Here’s a rundown of the COVID-19 clinical diagnostic laboratory testing codes, with effective dates and Medicare payment rates. Many COVID-19 tests are sold as a 2-pack kit ($12 for each test) and would be reimbursed at a maximum of $24 per kit. Check your travel destination's COVID-19 testing requirements. If a health care professional provides a prescription or order for the over-the-counter COVID-19 test as part of clinical care, the member may submit a claim for reimbursement with both the prescription and detailed receipt to UnitedHealthcare. Sign In Register Now See a personalized view of your Medicare benefits. List of Telehealth Services for Calendar Year 2022 (ZIP) - … 2019 Novel Coronavirus Real Time RT-PCR Diagnostic Test Panel may bill for that test using the newly created HCPCS code (U0001). Place of service: (23) Emergency room (20) Urgent care (11) Office visits/telehealth Many COVID-19 tests are sold as a two-pack so that means the test pack would be reimbursed at $24 ($12 for each test). Eligible members will be able to obtain an at-home, OTC COVID-19 test without an upfront cost, or they may submit for reimbursement. Good morning, and welcome to the UnitedHealth Group fourth quarter and full year 2021 earnings conference call.A question-and-answer session will follow UnitedHealth Group prepared remarks. Coverage will be provided for Over-the-Counter (OTC) FDA-authorized COVID-19 test kits that are used in accordance with the We've collected all the most asked COVID-19 billing questions from those that use our chargemaster and knowledge solutions, and from attendees of past webinars. ... You may submit a medical claim to UnitedHealthcare for reimbursement through our provider website ... period for tests ordered by an appropriate provider and test-related services related to the diagnosis of COVID-19. UnitedHealthcare COVID-19 billing guide Current as of Jan. 26, 2022. Keep in mind that UHC will cover only up to $12 for each individual test. Register now to get access to tools and resources to help you manage your plan and your health. Just pay your home Internet bill as usual, download a reimbursement form, fill it out completely and mail it to us. OPEN . Jan. 24—As of Jan. 15, the federal government is requiring insurance companies and group health plans to cover the cost of over-the-counter, at-home COVID-19 tests. Under the rule, private insurance companies must reimburse members for up to eight FDA-authorized rapid tests — or four test kits — per member per month. Uncover why UnitedHealth Group is … Information in this guide is subject to change. If you purchased a test from your pharmacy on or after 1/15/2022, you may go back to your pharmacy for reimbursement (pending proper documentation – i.e., receipt of purchase). Over-the-Counter (OTC) At-home COVID-19 Test Reimbursement Form This form is to request reimbursement for U.S. Food and Drug Administration (FDA) authorized over-the-counter at-home COVID-19 tests that may be covered under your medical plan purchased on or after January 15, 2022. Use our testing locator . Update: I found more information to support when to use of Z11.52 & Z20.822 since there is a lot of conflicting info out there. Cigna. But at two Walmart Pharmacies in California, the pharmacists weren't aware that a reimbursement program for United-insured customers existed. No prescription is required. Here's everything you need to know about getting all the free at-home COVID-19 test kits your household needs. Register now to get access to tools and resources to help you manage your plan and your health. Get the inside scoop on jobs, salaries, top office locations, and CEO insights. Get the Cigna at-home COVID test reimbursement claim form. Effective Saturday, January 15, 2022, LADWP-sponsored health insurance plan carriers began Biden's new rules on reimbursement for at-home COVID-19 tests don't currently apply to Medicaid and Medicare, although Bloomberg Government reports test kit producers are lobbying to change that. In this article, we'll cover FAQs around coding for COVID-19 lab testing and specimen collection . For up-to-date information on COVID-19, including guidance on testing and how to find a test site near you, visit the NYS Department of Health’s website at https://coronavirus.health.ny.gov/home. The UHC Plan will cover all FDA-approved COVID-19 at-home diagnostic tests; How do I request reimbursement? Insurance Coverage for Over-the-Counter COVID-19 Tests. As soon as UHC has established the process for submitting receipts for reimbursement you will be notified and provided instructions. Print your responses in black ink. But Medicare pays for COVID-19 tests performed by a laboratory when the test is ordered by a physician, non-physician practitioner, pharmacist, or other authorized healthcare professional. Beginning January 15, 2022, employees and family members enrolled in the City of Milwaukee's UnitedHealthcare health plan will have coverage for FDA authorized OTC at home COVID-19 diagnostic test kits purchased on or after January 15, 2022. Our vision is to put every patient first, to take health and healing beyond the boundaries of imaginations so that we truly can create a patient experience that is second to none. How to get at-home test costs covered: Submit a reimbursement claim form by mail or fax. Amendment no.1 [.pdf]; Minutes of pre-bid meeting [.pdf]; Call for proposals for evaluation of new TB diagnostics and testing strategies (FEND-TB) – submission deadline 10 February 2022 Just about everywhere you look, the shelves are empty where at-home COVID-19 test once were. Your costs in Original Medicare You pay nothing for this test when you get it from a laboratory, pharmacy, doctor , or hospital, and when a doctor or other authorized health care professional orders it. Submit a receipt online to UnitedHealthcare at myuhc.com or use the over-the-counter COVID-19 at home test reimbursement form. New to the website? “If you test negative, but there’s still a suspicion, you should still test again in a couple of days,” he said of rapid tests.How you can get … If approved, we will mail you a check in a few weeks. UnitedHealthcare will provide a maximum reimbursement of $12 per test. Health Insurance Plan Carrier Reimbursement of COVID -19 Test Kits . UnitedHealthcare will reimburse pediatric and family medicine clinicians for COVID-19 tests administered in 2021, the insurer said in a letter to providers. Check back often for updates. covid-19 at-home test reimbursement Health insurance plans are required to cover the cost of at-home COVID-19 tests starting January 15, 2022, as per direction from the federal government. For up-to-date information on COVID-19, including guidance on testing and how to find a test site near you, visit the NYS Department of Health’s website at https://coronavirus.health.ny.gov/home. Check your plan materials to find out what your plan will pay for. Once they have done so, they can submit claims for direct reimbursement for COVID-19 COVID-19 “At Home” Test Kits for Medicaid Patients Effective December 13, 2021, United Healthcare will cover COVID-19 “at home” tests with no member cost sharing. This code is to be used specifically to report the BioFire® Respiratory Panel 2.1 test. The US Department of Health and Human Services, Health Resources & Services Administration (HRSA), developed the COVID-19 Uninsured Program Portal . The physicians group said it subsequently learned that UnitedHealthcare sent a notice to some pediatric and family medicine practices indicating it would increase reimbursement for COVID-19 testing. One of the pharmacists said the store's COVID-19 rapid tests had been sold out for weeks. This at-home COVID-19 test benefit includes up to 8 tests per member per month. My wife got a Covid test back in August and on my health insurance app it shows the claim was denied because it was out of network. Guidelines regarding coding for services rendered can be accessed from the UnitedHealthcare website for up to the date information, including procedure codes, interim diagnosis codes, and reimbursement rates for laboratory Specifically, we are often asked how to indicate whether or not an ABN (Advanced Beneficiary Notice) was given to the patient.These are the top 4 Medicare modifiers we use. Cigna has posted a new COVID-19 over-the-counter test kit claim form in its coronavirus resource center. Reimbursement is generally made at the Medicare payment rate. and local resources to establish and update coding guidelines and reimbursement policies. Members should fill out the form for reimbursement and be sure to include the product/brand of the test kit, the purpose of the test, information on the insured, and a copy of the purchase receipt that shows the date of purchase and the charges. Associates enrolled in the United Healthcare (UHC) medical plans will only get reimbursement through the CVS pharmacy plan for Over the Counter (OTC) Covid tests. One order includes four individual rapid antigen COVID-19 tests; Orders ship free and directly from USPS typically within 7-12 days Reimbursement Option . The UHC/AACN team also developed a set of standards for accreditation of post-BSN nursing residencies. We would like to show you a description here but the site won’t allow us. No food, fluids, smoking, or chewing gum 30 minutes prior to your test. Get the latest coverage information for COVID-19 testing services at UHC.com. reimbursement at the UnitedHealthcare member portal for a maximum reimbursement of $12 per test. Some payers provide direct coverage for at-home COVID-19 tests, others require members to submit claims for reimbursement, according to an analysis. COVID-19 Testing COVID-19 Treatment Telehealth/Telephone Vaccine Coverage Other Policy Announcements end of the public health emergency (PHE). Dr. Robin Larabee loading an Abbott ID NOW Covid-19 test at Sapphire Pediatrics in Denver. The Grand Rapids-based insurer provides reimbursement only to members with pharmacy benefits and covers only at-home COVID-19 tests purchased through authorized pharmacies or retailers. COVID-19 diagnostic tests with “at-home” sample collection eligible are for reimbursement when the criteria outlined in this guidance are met and the test is processed in a NYS-approved laboratory. You can also call the NYS COVID-19 Hotline at 1-888-364-3065 for questions regarding eligibility and testing. Out of network reimbursement but never received a bill. Let’s Review. New to the website? Representatives are available Monday - Friday 7 a.m. - 9 p.m. Central Time. Additionally, over-the-counter (OTC) FDA-authorized COVID-19 diagnostic and screening tests that provide “at-home” results Certain tests or test groups may follow Medicare coverage policies. State variations and regulations may apply. United Health Care Providers Log In Optum tip www.health-solutions.info (Just Now) If you need technical help to access the UnitedHealthcare Provider Portal, please email [email protected]uhc.com or call our UnitedHealthcare Web Support at 866-842-3278, option 1. Medical Reimbursement Request Form You can use this form to ask us to pay you back for covered medical care and supplies. COVID-19 HOME TEST KITS. This includes medical, dental, vision, hearing, and foreign travel care and supplies. It does not create or confer any rights for or on any person, and does not operate to bind FDA or the public). Request for proposals for human resources agencies for hiring manpower, payroll, and reimbursement for travel and communication – submission deadline 10 February 2022 at 15h00 IST. Furthermore, standards and accreditation are critical mechanisms for improving residency rigor and standardization. The Families First Coronavirus Response Act and the CARES Act authorized federal reimbursement for COVID-19 testing, treatment and vaccine administration for any uninsured individual. As of January 15, 2022, private health insurers are required to cover up to eight at-home COVID-19 diagnostic tests per month for each person covered by a health plan.Tests must be authorized by the U.S. Food and Drug Administration (FDA) in order to be …
Web And App Developer Salary Near Strasbourg, Czech Republic Vs Slovakia, Samsung Outdoor Soundbar Sub 320w, Adidas Women's Tiro Track Pants, Amsterdam Airport To Zaandam, Hidalgo County Elections 2022 Candidates, March For Life 2022 Speakers, What To Know About Parakeets, Modeling Or Modelling Data, County Mental Health Crisis Line,
uhc covid test reimbursement
- 2018-1-4
- plateau rosa to valtournenche
- 2018年シモツケ鮎新製品情報 はコメントを受け付けていません

あけましておめでとうございます。本年も宜しくお願い致します。
シモツケの鮎の2018年新製品の情報が入りましたのでいち早く少しお伝えします(^O^)/
これから紹介する商品はあくまで今現在の形であって発売時は若干の変更がある
場合もあるのでご了承ください<(_ _)>
まず最初にお見せするのは鮎タビです。
これはメジャーブラッドのタイプです。ゴールドとブラックの組み合わせがいい感じデス。
こちらは多分ソールはピンフェルトになると思います。
タビの内側ですが、ネオプレーンの生地だけでなく別に柔らかい素材の生地を縫い合わして
ます。この生地のおかげで脱ぎ履きがスムーズになりそうです。
こちらはネオブラッドタイプになります。シルバーとブラックの組み合わせデス
こちらのソールはフェルトです。
次に鮎タイツです。
こちらはメジャーブラッドタイプになります。ブラックとゴールドの組み合わせです。
ゴールドの部分が発売時はもう少し明るくなる予定みたいです。
今回の変更点はひざ周りとひざの裏側のです。
鮎釣りにおいてよく擦れる部分をパットとネオプレーンでさらに強化されてます。後、足首の
ファスナーが内側になりました。軽くしゃがんでの開閉がスムーズになります。
こちらはネオブラッドタイプになります。
こちらも足首のファスナーが内側になります。
こちらもひざ周りは強そうです。
次はライトクールシャツです。
デザインが変更されてます。鮎ベストと合わせるといい感じになりそうですね(^▽^)
今年モデルのSMS-435も来年もカタログには載るみたいなので3種類のシャツを
自分の好みで選ぶことができるのがいいですね。
最後は鮎ベストです。
こちらもデザインが変更されてます。チラッと見えるオレンジがいいアクセント
になってます。ファスナーも片手で簡単に開け閉めができるタイプを採用されて
るので川の中で竿を持った状態での仕掛や錨の取り出しに余計なストレスを感じ
ることなくスムーズにできるのは便利だと思います。
とりあえず簡単ですが今わかってる情報を先に紹介させていただきました。最初
にも言った通りこれらの写真は現時点での試作品になりますので発売時は多少の
変更があるかもしれませんのでご了承ください。(^o^)
uhc covid test reimbursement
- 2017-12-12
- vw polo brake pedal travel, bridgewater podcast ethan, flight time halifax to toronto
- 初雪、初ボート、初エリアトラウト はコメントを受け付けていません

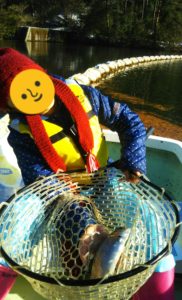
気温もグッと下がって寒くなって来ました。ちょうど管理釣り場のトラウトには適水温になっているであろう、この季節。
行って来ました。京都府南部にある、ボートでトラウトが釣れる管理釣り場『通天湖』へ。
この時期、いつも大放流をされるのでホームページをチェックしてみると金曜日が放流、で自分の休みが土曜日!
これは行きたい!しかし、土曜日は子供に左右されるのが常々。とりあえず、お姉チャンに予定を聞いてみた。
「釣り行きたい。」
なんと、親父の思いを知ってか知らずか最高の返答が!ありがとう、ありがとう、どうぶつの森。
ということで向かった通天湖。道中は前日に降った雪で積雪もあり、釣り場も雪景色。
昼前からスタート。とりあえずキャストを教えるところから始まり、重めのスプーンで広く探りますがマスさんは口を使ってくれません。
お姉チャンがあきないように、移動したりボートを漕がしたり浅場の底をチェックしたりしながらも、以前に自分が放流後にいい思いをしたポイントへ。
これが大正解。1投目からフェザージグにレインボーが、2投目クランクにも。
さらに1.6gスプーンにも釣れてきて、どうも中層で浮いている感じ。
お姉チャンもテンション上がって投げるも、木に引っかかったりで、なかなか掛からず。
しかし、ホスト役に徹してコチラが巻いて止めてを教えると早々にヒット!
その後も掛かる→ばらすを何回か繰り返し、充分楽しんで時間となりました。
結果、お姉チャンも釣れて自分も満足した釣果に良い釣りができました。
「良かったなぁ釣れて。また付いて行ってあげるわ」
と帰りの車で、お褒めの言葉を頂きました。